|
Case Report
Acalculous cholecystitis and ascites in a patient with rhabdomyolysis: A case report
1 Emergency Department, Security Forces Hospital, P.O. Box 3643, Riyadh City 11481, Kingdom of Saudi Arabia
Address correspondence to:
Yahia Akeely
MD, Emergency Department, Security Forces Hospital, P.O. Box 3643, Riyadh City 11481,
Kingdom of Saudi Arabia
Message to Corresponding Author
Article ID: 100108Z06IS2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Showaihi I, Akeely Y, Bokhari N, Saulat SR, Almalki N, Aldini M. Acalculous cholecystitis and ascites in a patient with rhabdomyolysis: A case report. Case Rep Int 2022;11(2):1–4.ABSTRACT
Introduction: Rhabdomyolysis is a muscle breakdown caused by a variety of factors. Based on a review of the literature, we are unaware of any case reports that discuss these complications of rhabdomyolysis with acalculous cholecystitis and ascites.
Case Report: This patient is a 24-year-old man who had never had a chronic illness before. He was a nonsmoker and did not consume alcoholic beverages. He went to the emergency room (ER) because he was having upper abdominal pain and aches throughout his body. He was just started a rigorous physical activity-based training regimen. A total creatine kinase (CK) level more than 5 times higher than the upper normal value confirmed the diagnosis. For the upper abdominal pain, an ultrasound was performed. It reveals ascites and a thick-walled gallbladder. With a decrease in repeated total CK and clinical improvements, the patient was discharged home after aggressive hydration. The patient was asymptomatic at the follow-up appointment, and the ultrasound showed no ascites or gallbladder wall thickness.
Conclusion: These are a rare complication of rhabdomyolysis. It implies that acalculous cholecystitis and ascites should be interpreted in light of the clinical scenario and presentation. The workup for ascites and acalculous differential diagnosis was uneventful. In a young patient with rhabdomyolysis, acalculous cholecystitis and ascites is an unusual occurrence.
Keywords: Acalculous cholecystitis, Ascites, Rhabdomyolysis
INTRODUCTION
Rhabdomyolysis is a clinical syndrome characterized by skeletal muscle destruction and the release of intracellular muscle contents into the bloodstream [1]. The definition of rhabdomyolysis varies, but most references agree on 5 times the upper normal level of total CK [2]. Rhabdomyolysis can be caused by different conditions. One of the known causes is strenuous exercise [3],[4]. The definitive treatment is aggressive hydration, which is supported by the majority of references and guidelines [5]. Furthermore, there are several treatment options that are still controversial, such as sodium bicarbonate, mannitol, acetazolamide, and furosemide [6]. There may be a need for hemodialysis in certain circumstances. Complications of rhabdomyolysis include compartment syndrome, electrolyte disturbances, cardiac arrhythmia, renal failure, and disseminated intravascular coagulation. To avoid such complications, we should treat it aggressively with intravenous fluid hydration. The electrolytes and electrocardiogram (ECG) should be closely monitored.
There is no universal fluid replacement guideline; it varies from one reference to the next and from one guideline to the other. The majority of them agreed to keep urine output at 300 mL/h. Similarly, there is no evidence to support a particular type of fluid, such as normal saline versus lactated ringer or colloids [7].
Acalculous cholecystitis can be caused by a variety of factors [8],[9],[10]. Known precipitating factors include severe sepsis, intensive care unit (ICU) patients, burns, long starvation, total parental nutrition, and trauma [11],[12],[13]. No case report that we are aware of mentions rhabdomyolysis as a cause of acalculous cholecystitis. Ascites, on the other hand, has a variety of causes [14],[15]. Rhabdomyolysis was not mentioned as a cause in any of the case reports.
CASE REPORT
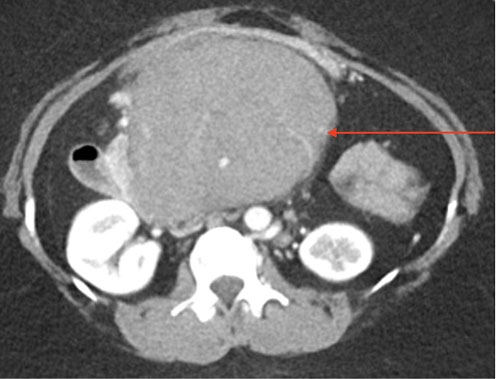
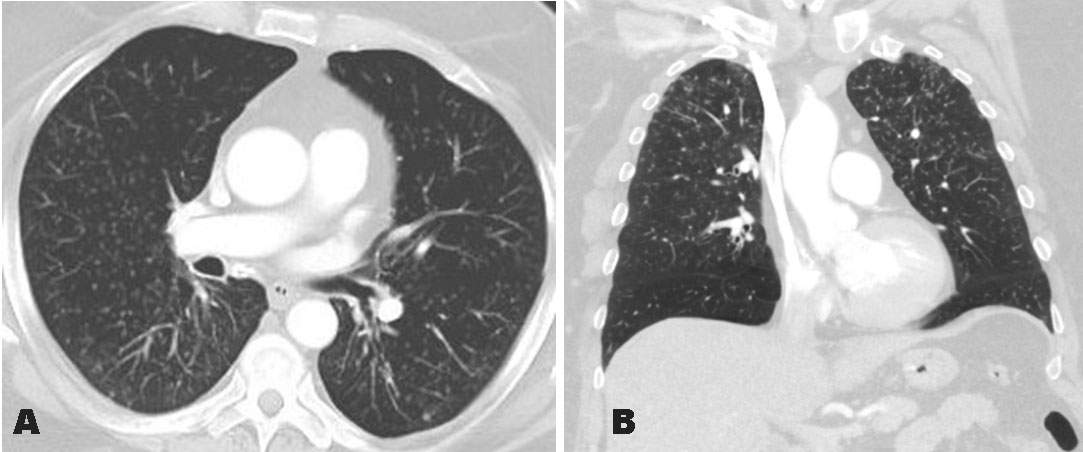
This is a young healthy patient not known to have medical illnesses before; referred from another medical institution as a case of strenuous exercise-induced rhabdomyolysis. The patient was complaining of generalized body aches and upper abdominal pain after a heavy exercise for few days prior to presentation; no chest pain, no fever, no trauma. On arrival to our department, these were the vital signs; blood pressure (BP) 138/80, heart rate (HR) 85, respiration rate (RR) 18, saturation 98% on room air, and temperature 36.6 °C. On physical examination; the patient was fully conscious, no jaundice, average weight, not in respiratory distress. Chest and cardiovascular examination was normal. The abdominal examination showed only mild tenderness right upper quadrant and epigastric areas. The blood work was done. It showed normal white blood count (WBC), platelet, hemoglobin, aspartate transaminase (AST), alanine aminotransferase (ALT), and albumin. Furthermore, the urea and creatinine were within normal. The total creatine kinase (CK) was more than 5 times the upper limit (2441 U/L). Since the patient was having upper abdominal pain, ultrasound bedside done and it showed ascites (Figure 1) and gallbladder wall-thickness with a pericholecystic free fluid (Figure 2). The patient was admitted in the emergency department for management and close observation. He stayed around 29 hours. The total amount of fluid received in the 1st 16 hours is 11 liters. In the next 13 hours, he received 2.6 liters of normal saline as boluses of 500 mL and 1 liter.
The patient was monitored clinically, and the CK was followed serially. The CK was reduced and reached 1090 U/L just before discharge. The bedside echocardiography was within normal.
On a booked revisit after a week, the patient was asymptomatic, no abdominal pain, with normal bedside ultrasound. There was no ascites or gallbladder thickness (Figure 3).
DISCUSSION
Acalculous cholecystitis and ascites are unusual consequences of rhabdomyolysis. The main treatment of rhabdomyolysis is aggressive hydration to avoid renal injury and complications. On the other hand, rhabdomyolysis results in muscle cell breakdown, with the release of toxic contents into the extracellular space and damage to adjacent capillaries, which lead to edema [16]. This could be the reason for acute acalculous cholecystitis and ascites.
The amount of fluid should be closely observed and monitored. The urine output should be measured and usually it should target ~300 mL/h [17]. All signs of volume overload such as difficulty breathing, edema in the face or extremities, should be recorded. This patient has no other reason for the ascites or cholecystitis other than as a complication of strenuous exercise and rhabdomyolysis.
The abdomen’s free fluid must be investigated. If the likely etiology is not evident, blood tests and fluid analysis should be performed. In this case, the presentation is consistent with that of exercise-induced rhabdomyolysis. Despite this, basic search and examinations into other possible causes, such as infections, heart failure, liver injury, low albumin, and renal issues, have been undertaken, see Table 1 for common causes of ascites and acalculous cholecystitis. Everything was within the normal range.
Other than the underlying rhabdomyolysis, there are no other clear reasons of the ascites. In addition, the treating physician requests that the patient be followed up. During the follow-up, no new ascites were identified, and the patient did well.
On the other hand, several causes of acalculous cholecystitis were investigated. There were no other explanations for the existence of acalculous cholecystitis. On the scheduled follow-up, there was no further acalculous cholecystitis.
CONCLUSION
We discuss an uncommon complication of rhabdomyolysis caused by intense activity in this patient. Ascites and acalculous cholecystitis can occur in rhabdomyolysis. This is an uncommon problem that has never been documented in the literature before. In such cases, aggressively treat rhabdomyolysis with fluids and monitor the patient on a frequent basis. In this case the patient’s recovery went well.
REFERENCE
1.
Chavez LO, Leon M, Einav S, Varon J. Beyond muscle destruction: A systematic review of rhabdomyolysis for clinical practice. Crit Care 2016;20(1):135. [CrossRef]
[Pubmed]

2.
Stahl K, Rastelli E, Schoser B. A systematic review on the definition of rhabdomyolysis. J Neurol 2020;267(4):877–82. [CrossRef]
[Pubmed]

3.
Manspeaker S, Henderson K, Riddle D. Treatment of exertional rhabdomyolysis in athletes: A systematic review. JBI Database System Rev Implement Rep 2016;14(6):117–47. [CrossRef]
[Pubmed]

4.
Tazmini K, Schreiner C, Bruserud S, Raastad T, Solberg EE. Exercise-induced rhabdomyolysis – A patient series. Tidsskr Nor Laegeforen 2017;137(21). [CrossRef]
[Pubmed]

5.
Long B, Koyfman A, Gottlieb M. An evidence-based narrative review of the emergency department evaluation and management of rhabdomyolysis. Am J Emerg Med 2019;37(3):518–23. [CrossRef]
[Pubmed]

6.
Cabral BMI, Edding SN, Portocarrero JP, Lerma EV. Rhabdomyolysis. Dis Mon 2020;66(8):101015. [CrossRef]
[Pubmed]

7.
Scharman EJ, Troutman WG. Prevention of kidney injury following rhabdomyolysis: A systematic review. Ann Pharmacother 2013;47(1):90–105. [CrossRef]
[Pubmed]

8.
9.
10.
11.
Jones MW, Ferguson T. Acalculous Cholecystitis. 2022 Apr 13. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2021.
[Pubmed]

12.
13.
14.
Tsochatzis EA, Gerbes AL. Diagnosis and treatment of ascites. J Hepatol 2017;67(1):184–5. [CrossRef]
[Pubmed]

15.
Oey RC, van Buuren HR, de Man RA. The diagnostic work-up in patients with ascites: Current guidelines and future prospects. Neth J Med 2016;74(8):330–5.
[Pubmed]

16.
17.
McKinney B, Gaunder C, Schumer R. Acute exertional compartment syndrome with rhabdomyolysis: Case report and review of literature. Am J Case Rep 2018;19:145–9. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Ibrahim Showaihi - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Yahia Akeely - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Nader Bokhari - Acquisition of data, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Swaid Raza Saulat - Conception of the work, Design of the work, Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Naif Almalki - Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mohammed Aldin - Acquisition of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 Ibrahim Showaihi et al.. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.