|
Case Report
Adenoid cystic carcinoma of the nasal cavity—the great mimicker of chronic rhinitis: A rare case report with literature review
1 Senior Resident, Department of Pathology, Makerere College of Health Sciences, Kampala, Uganda
2 Tutorial Assistant, Department of Anatomy and Histology, College of Health Sciences, University of Dodoma, Dodoma, Tanzania
3 Lecturer, Department of Surgery, University of Dodoma, Dodoma, Tanzania
Address correspondence to:
James Yahaya
Department of Pathology, Makerere College of Health Sciences, P.O. BOX 7072, Kampala,
Uganda
Message to Corresponding Author
Article ID: 100067Z06JY2019
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Yahaya J, Abraham Z. Adenoid cystic carcinoma of the nasal cavity—the great mimicker of chronic rhinitis: A rare case report with literature review. Case Rep Int 2019;8:100067Z06JY2019.ABSTRACT
Introduction: Adenoid cystic carcinoma (ACC) of the nasal cavity is one of the rarest malignant entities reported in the literature with the known incidence of up to 5%. It commonly poses a diagnostic challenge due to lack of diagnostic suspicion index because of its rarity and especially when it is associated with a long history of benignity. Adenoid cystic carcinoma is a tumor of salivary glands even though it is not frequent. Moreover, it can rarely occur in other body parts, such as nose, paranasal sinuses, lungs, uterine cervix, and many others.
Case Report: We present a case of an 18-year-old boy with a diagnosis of ACC of the nasal cavity. The patient had a 10-year history of long-standing chronic inflammatory condition presenting as rhinitis. However, after a period of two years later following the initial diagnosis, the tumor became aggressive and it presented with ulceration, causing erosion of the nasal bone as well as auto-exenteration of the right eye.
Conclusion: Adenoid cystic carcinoma involving the nose and other paranasal sites ought to be deemed as a tumor with sometimes long-standing history of benignity which needs high index of suspicion for being able to detect it in order to improve outcome of the patients.
Keywords: Adenoid cystic carcinoma, Nose
INTRODUCTION
Adenoid cystic carcinoma (ACC) accounts for approximately 10% of salivary gland tumors [1],[2]. It accounts for 3–5% of all head and neck malignancies [3]. When ACC involves the paranasal sinuses, the maxillary sinus is the most common site followed by the nasal cavity especially the lateral wall, as reported in most of the literatures [4]. For this reason, ACC arises from pseudostratified columnar epithelium rather than the glandular tissue of salivary glands [4]. This can be explained by the fact that ACC is not only confined to the salivary glands, but it tends to develop even in other sites in which there is pseudostratified columnar epithelium.
CASE REPORT
An 18-year-old boy presented in the ear, nose, and throat (ENT) clinic with a large ulcerating and erosive midline lesion involving the nasal cavity and the right eye for almost 10 years. The patient presented initially with episodes of recurrent rhinitis. The swelling was progressively increasing in size and later on it started ulcerating and it was extending to involve other parts of the nose, face, and the right eye (Figure 1).
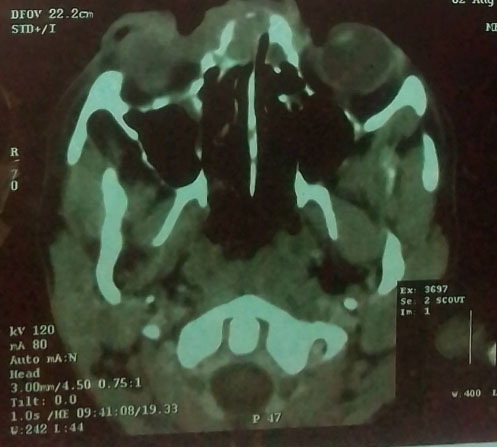
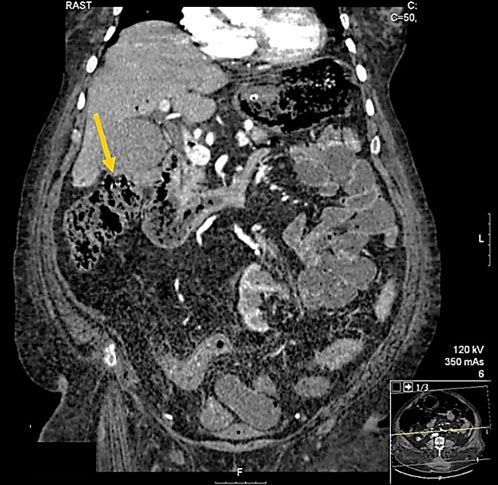
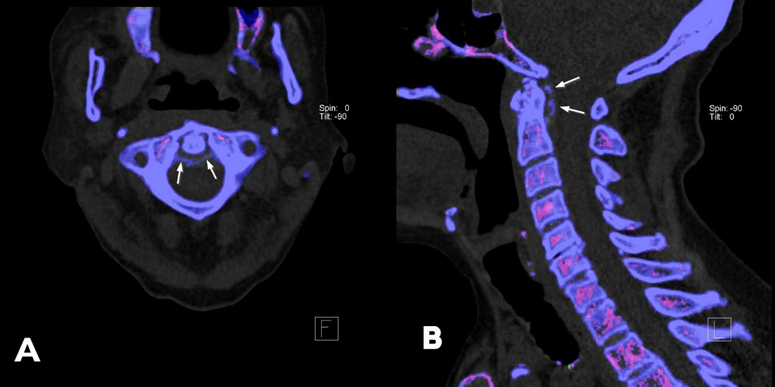
This was followed by nasal blockage, copious purulent nasal discharge mixed with blood for some time. Eight years later as the condition became more severe, he went to one of the health facilities where a computed tomography (CT) scan was done which showed an extensive tumor causing erosion of the nasal bone and extending to the right orbital rim (Figure 2).
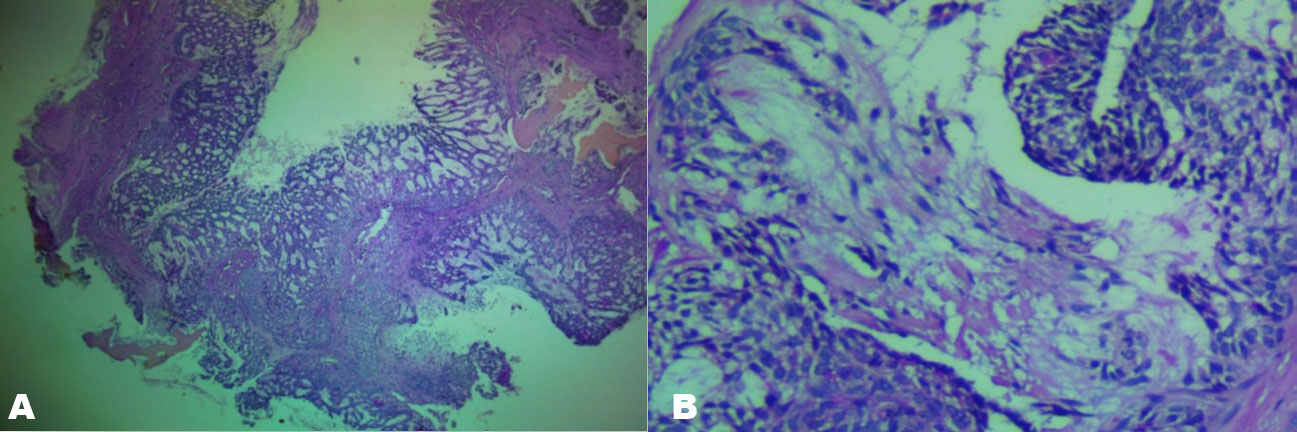
An incisional biopsy was taken and the histological result revealed a benign skin appendage tumor. He went back home in the village and he did not make any followup for a period of about two years. Then he developed hemiplegia due to paralysis of both lower limbs, episodes of severe headache mainly in the frontal side of the head and auto-exenteration of the right eye. He also reported right-sided hearing loss without otorrhea. A second incisional tissue biopsy was taken from the tip of the right nasal wall. The histological findings showed small fragments of tissue sections infiltrated by a tumor which was composed of pseudoglandular structures with cystic appearance and nests of blending darkly stained nuclear tumor cells giving a cribriform pattern was seen. A diagnosis of ACC of the nasal bone was made (Figure 3A). The tumor had invaded nerves in some areas (Figure 3B). The tumor was staged as a Stage IV tumor (T4N0M0).
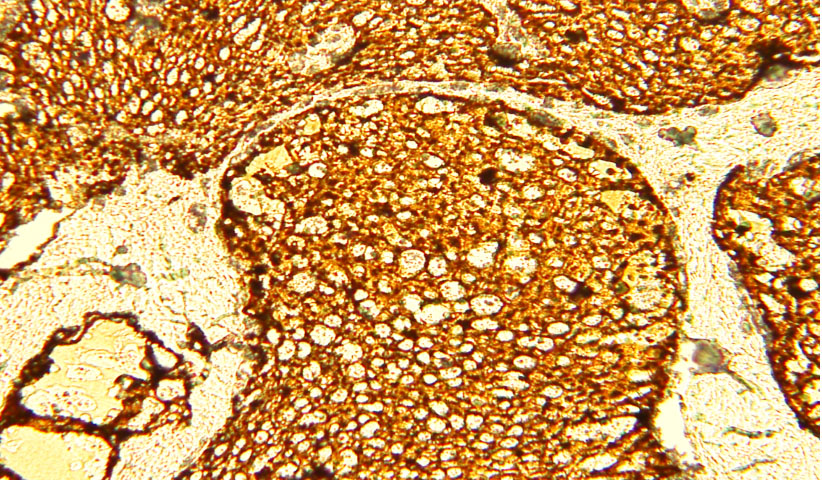
Immunohistochemistry (IHC) staining for S-100 antigen was diffuse and strongly positive (Figure 4). Ki67 proliferation labeling index (LI) was low (6%) based on the cut-off point of 10% and P53 staining was negative.
The patient did not want to start any treatment. Therefore, he consented for denying treatment and he was discharged. He died after three months after we had enquired from his relatives through the phone number they had given us.
DISCUSSION
The age of the patients ranges from 20 to 84 years with a median age of 52 years having a higher preponderance in females compared to males with a ratio of 2:1 [5],[6]. There are no known risk factors or etiological agents for both familial and sporadic ACC. A number of cases with ACC have been found with distinctive chromosomal translocation t(6;9) (q22–23;p23–24), which results in fusion of MYB gene and NFIB gene found on chromosome 6 and 9, respectively; this fusion of the two genes leads to abnormal proliferation of the cells involved in the process [7].
Clinically, patients commonly present with nasal blockage [6],[8] as it was for the patient in this case report. Nasal blockage can result from mass, swelling of the cheek and polyps. Other clinical presentations found in patients with nasal ACC are epistaxis, nerve symptoms, and visual symptoms which may present as blurred vision, exophthalmos, proptosis, ptosis, diplopia, or decreased vision [5],[6],[7]. Headache, hearing problems, and nerve symptoms, such as paralysis, have also been reported widely in the English literature [8],[9].
Therefore, when there are repeated episodes of features, such as rhinitis and epistaxis, taking imaging of the nasal and paranasal areas ought to be put in mind. This will help to rule out presence of ACC and other tumors. Histologically, ACC involving any anatomical site exists in three different morphological types including cystic, cribriform, and solid types. The histological growth pattern for the patient in this case report was of cribriform type.
Different treatment options have been reported in the literature. The common approach for treating sinonasal ACC includes surgery, radiotherapy, and chemoradiotherapy [1]. However, studies have shown that surgery alone carries better clinical outcome compared to either radiotherapy or chemoradiotherapy alone [9]. Surgery has also been found to delay recurrence which is the notorious biological behavior of ACC having 65–95% chances of developing even after surgery followed by radiotherapy [10],[11]. In addition, surgery has been reported to prevent recurrence and not just delaying its occurrence [9]. Quite a large number of prognostic factors have been reported to have influence on the clinical outcome of patients with nasal cavity ACC. The cribriform and cystic forms are the commonest histological types and they carry good prognosis compared to the solid type which is also rare [8]. Location of ACC to the head and neck has been found to influence the prognosis. Those involving maxillary sinus carry the worst prognosis after those involving the nasal bone due to bone infiltration and challenges to surgery [12]. Lymph node involvement plays a major role in determining the prognosis of ACC involving the salivary glands. However, it has also been argued that, even in patients with sinonasal ACC, dissection of neck lymph nodes confers improvement in prognosis of the patients [13]. Perineural invasion, surgical margins, and staging also help to determine the prognosis of patients with nasal cavity ACC. Elavarasi and colleagues reported that T3 and T4 tumors are associated with much higher incidence of perineural invasion compared to T1 and T2 tumors (60% vs. 23.5%) [14].
CONCLUSION
Adenoid cystic carcinoma of the nasal cavity may mimic other inflammatory conditions hence advance without being noticed. The association between xeroderma pigmentosa syndrome with adenoid cystic carcinoma requires molecular studies involving multiple cases in order to draw conclusion.
REFERENCE
1.
3.
4.
Lupinetti AD, Roberts DB, Williams MD, et al. Sinonasal adenoid cystic carcinoma: The M. D. Anderson Cancer Center experience. Cancer 2007;110(12):2726–31. [CrossRef]
[Pubmed]

5.
Rahmani K, Taghipour Zahir S, Baghi Yazdi M, Navabazam A. Aggressive adenoid cystic carcinoma of maxillary sinus in a 43-year-old male: Rare case report and review of literature. Case Rep Med 2017;2017:2324717. [CrossRef]
[Pubmed]

6.
Sanghvi S, Patel NR, Patel CR, Kalyoussef E, Baredes S, Eloy JA. Sinonasal adenoid cystic carcinoma: Comprehensive analysis of incidence and survival from 1973 to 2009. Laryngoscope 2013;123(7):1592–7. [CrossRef]
[Pubmed]

7.
Persson F, Fehr A, Sundelin K, Schulte B, Löning T, Stenman G. Studies of genomic imbalances and the MYB-NFIB gene fusion in polymorphous low-grade adenocarcinoma of the head and neck. Int J Oncol 2012;40(1):80–4. [CrossRef]
[Pubmed]

8.
Thompson LD, Penner C, Ho NJ, et al. Sinonasal tract and nasopharyngeal adenoid cystic carcinoma: A clinicopathologic and immunophenotypic study of 86 cases. Head Neck Pathol 2014;8(1):88–109. [CrossRef]
[Pubmed]

9.
10.
11.
Garden AS, Weber RS, Morrison WH, Ang KK, Peters LJ. The influence of positive margins and nerve invasion in adenoid cystic carcinoma of the head and neck treated with surgery and radiation. Int J Radiat Oncol Biol Phys 1995;32(3):619–26. [CrossRef]
[Pubmed]

12.
13.
Charlton P, Pitkin L. Airway compromise due to adenoid cystic carcinoma obstructing the distal trachea: A review of current management and clinical trials. BMJ Case Rep 2015;2015. pii: bcr2014204063. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgement
The authors would like to show appreciation for the relatives of the patient, radiologist, and the ENT surgeons for devoting their cooperation to give information which was highly needed for the preparation of this case report.
Author ContributionsJames Yahaya - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Zephania Abraham - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2019 James Yahaya et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.