|
Case Report
Morgagni–Stewart–Morel syndrome: A new case
1 (Dr). Endocrinology Diabetes and Metabolic Diseases Department, Avicenna Military Hospital, Marrakesh, Morocco
2 (Pr). Endocrinology Diabetes and Metabolic Diseases Department, Avicenna Military Hospital, Marrakesh, Morocco
Address correspondence to:
Lahoussaine Abainou
(Dr). Endocrinology Diabetes and Metabolic Diseases Department, Avicenna Military Hospital, Marrakesh,
Morocco
Message to Corresponding Author
Article ID: 100070Z06LA2019
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Abainou L, El Jadi H, El Hadri S, Baizri H. Morgagni–Stewart–Morel syndrome: A new case. Case Rep Int 2019;8:100070Z06LA2019.ABSTRACT
Introduction: Morgagni–Stewart–Morel (MSM) syndrome is defined as the presence of hyperostosis frontalis interna (HFI) associated with metabolic, endocrine, and neuropsychiatric disorders. Here, we present an MSM syndrome case involving a woman with symptoms of depression and infertility.
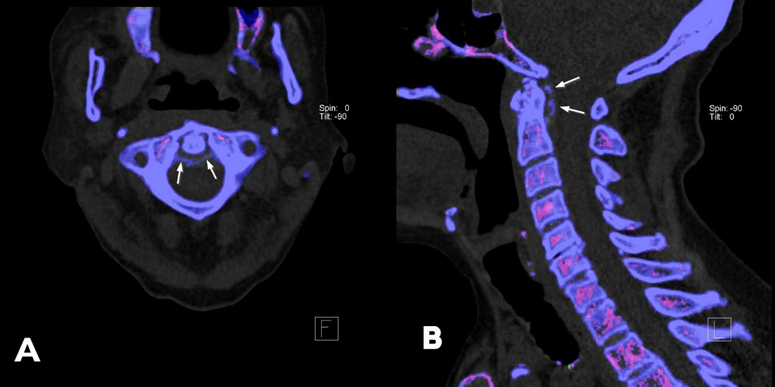
Case Report: A 38-year-old woman admitted for inaugural diabetic ketosis and she reported a history of severe frontal headache of which she had suffered for several years associated to depression, obesity, and infertility. Axial cranial computed tomography (CT) scan showed bilateral thickening of the inner table of the frontal bone. Her endocrine dysfunctions and neuropsychiatric symptoms are interpreted as components of Morgagni–Stewart–Morel syndrome and may correlate with the severity of the frontal hyperostosis and the cortical atrophy.
Conclusion: We describe a case of MSM syndrome, presenting many of the clinical features described in the literature. The exact etiology of HFI and MSM syndrome remains unclear; the most interesting theories relate to estrogen dysfunction, obesity and leptin dysfunction, and genetics.
Keywords: Endocrine and neuropsychiatric disorders, Hyperostosis frontalis interna, Morgagni–Stewart–Morel syndrome
INTRODUCTION
Morgagni–Stewart–Morel syndrome is an association of clinical features with radiological findings (HFI). The common clinical features are headache (migrainous), psychotic symptoms, metabolic and endocrine disorders (obesity, diabetes mellitus, and thyroid disease), hirsutism, osteoporosis, and menstrual disorders, but these associations are mostly based on case reports, and no clear consensus exists on the definition of the syndrome.
CASE REPORT
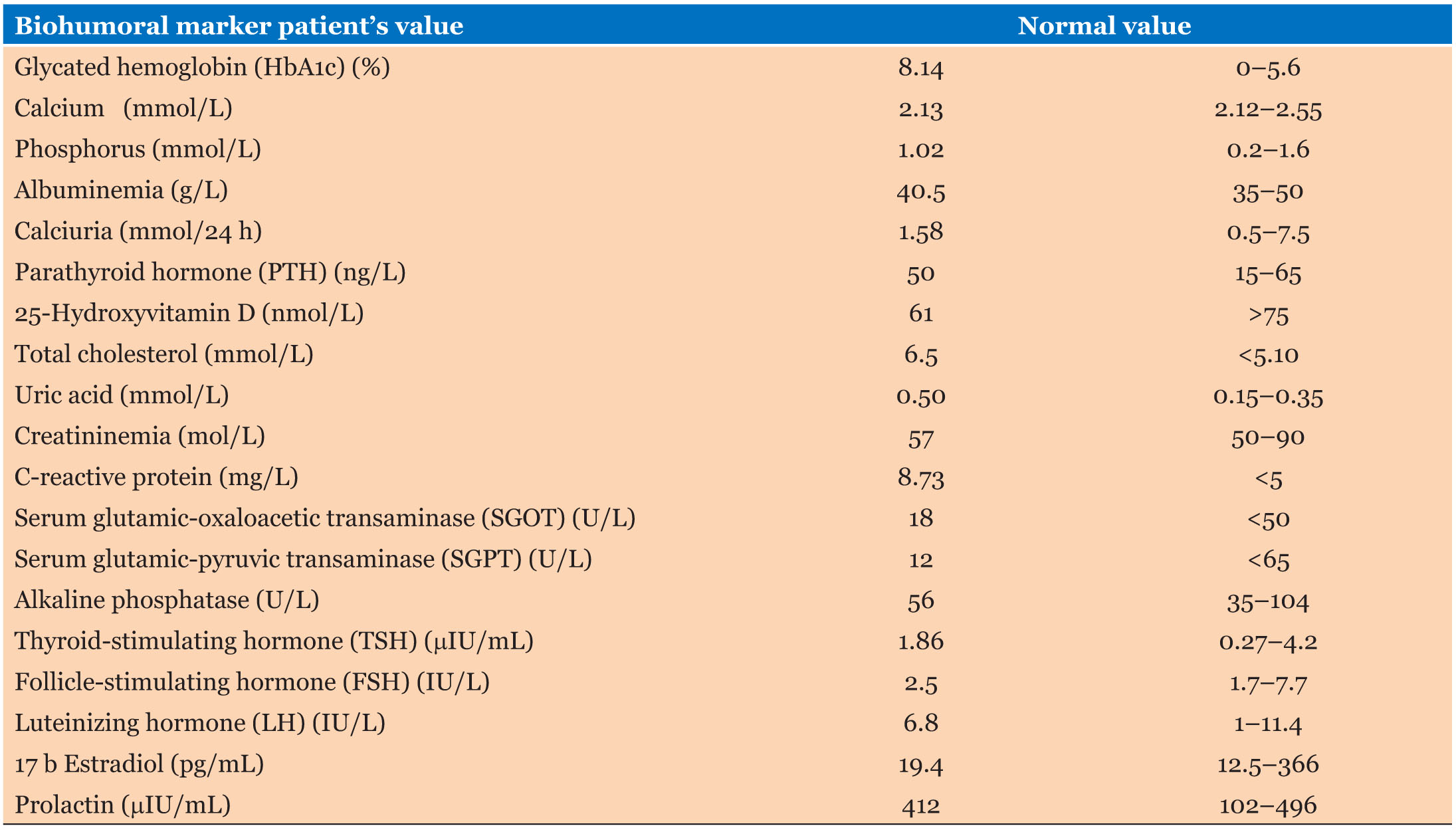
A 38-year-old woman, married without children, admitted in February 2019 to the Endocrinology Department for an inaugural diabetic ketosis. During the interrogation the patient complained that she had an eight-year history of severe chronic headaches never explored and she was being followed up by a psychiatrist for depression. She also reported a medical history of obesity, infertility for several years. On examination she was obese, depressed, and her body mass index (BMI) was 36 kg/m2. Axial cranial CT scan showed bilateral thickening of the inner table of the frontal bone (Figure 1A) and (Figure 1B). Lab values are given in Table 1.
These endocrine dysfunctions and neuropsychiatric symptoms are interpreted as components of MSM syndrome. For the severe headache, the surgical indication was discussed with the neurosurgeons but the patient refused immediately surgery and she was treated by analgesics with improvement under tramadol.
DISCUSSION
Morgagni–Stewart–Morel syndrome was first described in 1719 by Giovanni Battista Morgagni in an obese female patient during autopsy who had hirsutism and HFI defined as thickening of inner table of a skull [1].
The modern concept of its clinical significance was initiated in 1928 after Stewart reported three cases of the syndrome diagnosed at autopsy. The first living case was reported by Morel in 1930 [2],[3].
Hyperostosis frontalis interna is a morphological pattern of the frontal bone that is usually an incidental finding in X-ray, cranial computed tomography (CCT), or magnetic resonance imaging (MRI) studies [4].
Morgagni–Stewart–Morel syndrome is defined as the association of HFI with metabolic, endocrine, and neuropsychiatric disorders. But these associations are mostly based on case reports, and no clear consensus exists on the definition of the syndrome [4].
The etiology and pathogenesis behind skull thickening and MSM syndrome are till now not clear; the most interesting theories relate to extended exposure to estrogen, obesity and elevated leptin level, and genetics [5],[6].
The common clinical features are headache, hirsutism, menstrual disorders, galactorrhoea, obesity, diabetes mellitus, depression, irritability, fatigability, transitory hemiplegias, hearing impairment, cranial nerve palsies, muscle weakness, and seizures [7],[8],[9].
The treatment is generally symptomatic but there is a case of MSM syndrome described in the literature with violent headaches predominant in the clinical course treated surgically and the pain ceased immediately after the operation. The authors discuss surgical treatment especially in cases with high intensity headaches [10].
Morgagni–Stewart–Morel syndrome is also called as metabolic craniopathy due to its wide range of symptoms and endocrinal dysfunctions [11].
CONCLUSION
The known symptoms of MSM syndrome are mostly based on case reports, and they tend to be nonspecific. Patient with MSM syndrome may present varied symptoms associated to thickening of the inner table of the frontal bone, thus lead to difficulty in diagnosis.
REFERENCE
3.
Stewart RM. Localized cranial hyperostosis in the insane. J Neurol Psychopathol 1928;8(32):321–31. [CrossRef]
[Pubmed]

4.
Attanasio F, Granziera S, Giantin V, Manzato E. Full penetrance of Morgagni-Stewart-Morel syndrome in a 75-year-old woman: Case report and review of the literature. J Clin Endocrinol Metab 2013;98(2):453–7. [CrossRef]
[Pubmed]

5.
Rühli FJ, Henneberg M. Are hyperostosis frontalis interna and leptin linked? A hypothetical approach about hormonal influence on human microevolution. Med Hypotheses 2002;58(5):378–81. [CrossRef]
[Pubmed]

6.
Koller MF, Papassotiropoulos A, Henke K, et al. Evidence of a genetic basis of Morgagni-Stewart-Morel syndrome. A case report of identical twins. Neurodegener Dis 2005;2(2):56–60. [CrossRef]
[Pubmed]

7.
Capraro VJ, Dillon WP, Calabrese JS. Morgagni's syndrome: Metabolic craniopathy. Obstet Gynecol 1970;35(4):565–9.
[Pubmed]

8.
Hasegawa T, Ito H, Yamamoto S, Haba K, Murata H. Unilateral hyperostosis frontalis interna: A case report. J Neurosurg 1983;59(4):710–3. [CrossRef]
[Pubmed]

9.
Kishore B, Singh MM, Seth HC, Hazra DK, Trehon OP, Prakash C. Morgagni's syndrome: A case report. J Indian Med Assoc 1972;58(10):376–8.
[Pubmed]

10.
Latka D, Szydlik W, Glaubic-Latka M, Mrówka R. A case of Morgagni-Morel-Stewart syndrome with violent headaches predominant in the clinical course treated surgically. [Article in Polish]. Neurol Neurochir Pol 1995;29(2):253–6.
[Pubmed]

11.
Nallegowda M, Singh U, Khanna M, Yadav SL, Choudhary AR, Thakar A. Morgagni Stewart Morel syndrome – Additional features. Neurol India 2005;53(1):117–9.
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Lahoussaine Abainou - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Hamza El Jadi - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Sanae El Hadri - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Hicham Baizri - Conception of the work, Design of the work, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2019 Lahoussaine Abainou et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.