|
Case Report
Ileoileal intussusception due to metastatic melanoma
1 MBBS, Department of Surgery, Toowoomba Hospital, Queensland, Australia
2 MBBS, MSc, FRCSI, FRACS, Department of Surgery, Toowoomba Hospital, Queensland, Australia
Address correspondence to:
Ho Nam Choi
Toowoomba Hospital, Pechey Street, Toowoomba, Queensland 4350,
Australia
Message to Corresponding Author
Article ID: 100072Z06HC2019
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Choi HN, Arafat Y, Antoun I. Ileoileal intussusception due to metastatic melanoma. Case Rep Int 2019;8:100072Z06HC2019.ABSTRACT
Introduction: Intussusception in adults is rare, and can be classified into intussusception with a pathological lead point, or intussusception without a lead point.
Case Report: This case report describes a 63-year-old male with a history of metastatic melanoma who presented with a two-month history of abdominal pain, which was due to an ileoileal intussusception with metastatic melanoma deposit at the lead point. He was managed with laparoscopic small bowel resection, leading to resolution of his symptoms.
Conclusion: A low threshold for surgical exploration is recommended in adults with intussusception for definitive diagnosis of the cause and for symptom management.
Keywords: Intussusception, Laparoscopic surgery, Melanoma, Small intestine
INTRODUCTION
Intestinal intussusception, or the telescoping of a segment of bowel (intussusceptum) into adjacent segment of bowel (intussuscipiens), is a rare condition in adults which is responsible for 1–5% of bowel obstructions [1],[2]. While intussusception is relatively more common in the pediatric population, it is estimated that only about 5% of intussusception occur in adults [3], with an estimated incidence of 2–3 cases per 1,000,000 person-years [4]. Adult intussusception also differs from pediatric intussusception in its etiology and clinical presentation. Adult cases are more likely to present with milder and subacute or chronic symptoms, compared to those in children [5]. In children, intussusception is usually idiopathic and is thought to be often associated with enlargement of Peyer’s patches [5]. In contrast, adult intussusception is less often idiopathic in its etiology, and is more often associated with a presence of a pathological lesion in the lead point, which may be benign or malignant [5]. Benign lesions can include Meckel’s diverticulum, venous malformations, polyps, or lipomas, and malignant causes include adenocarcinoma and lymphomas [6]. Here, we present a case of a 63-year-old male patient who presented with ileoileal intussusception secondary to a metastatic melanoma deposit at the lead point. He underwent laparoscopic small bowel resection and anastomosis for symptom control.
CASE REPORT
A 63-year-old male with a history of metastatic melanoma was referred to the General Surgery team from Medical Oncology outpatient clinic. He was initially diagnosed with a cutaneous malignant melanoma of his back five years prior to this presentation, where he underwent a wide local excision of the primary lesion together with sentinel lymph node biopsy, followed by right axillary lymph node dissection. He was diagnosed with metastatic recurrence of his BRAF wild-type melanoma with hepatic, pulmonary, and hilar lymph node and pelvic sidewall lymph node metastases three years following the surgery. He was subsequently commenced on checkpoint inhibition immunotherapy with combined Ipilimumab and Nivolumab.
He had been reporting a two-month history of intermittent colicky central abdominal pain accompanied with alternating diarrhea and constipation. He did not have any nausea or vomiting, and there were no changes to his appetite or to his weight over the two months. He had not noticed any frank per rectal bleeding or melena.
On review by the surgical team, the patient was a slim Caucasian male who was asymptomatic at time of review. On physical examination, he had normal vital signs with a pulse rate of 80 beats per minute, blood pressure of 120/70 mmHg, respiratory rate of 18 breaths per minute with oxygen saturation of 98% on room air. He was afebrile with a temperature of 36.8°C. His abdomen was not distended. Palpation of his abdomen did not reveal any tenderness or masses. He had normal bowel sounds to auscultation.
Blood tests showed hemoglobin of 102 g/L, consistent with anemia, and a normal white cell count of 7.7 × 109/L. His serum electrolytes, renal function, and liver function tests were unremarkable.
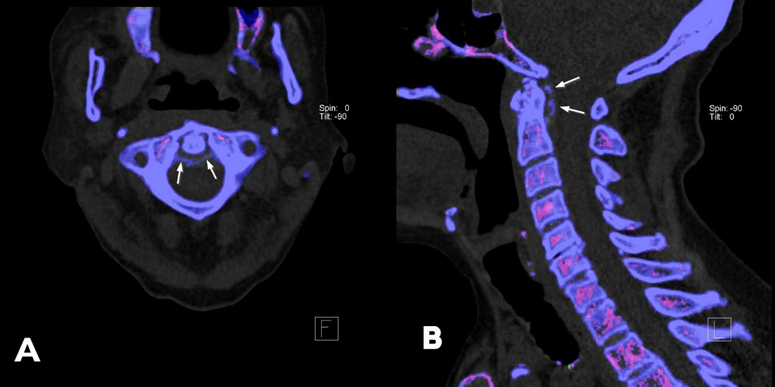
He was further investigated with a computed tomography (CT) enterography which demonstrated a small bowel intussusception with a 2.4 cm ileal lesion as the lead point (Figure 1). There was no radiological evidence of obstruction.
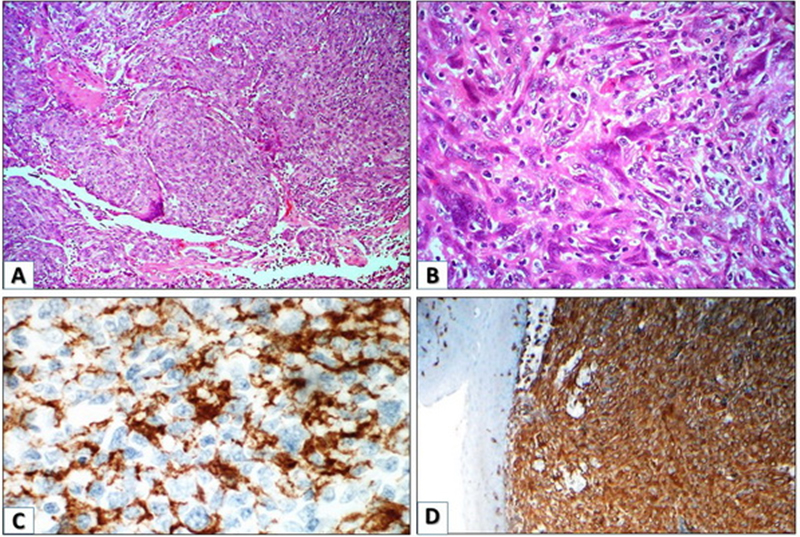
Based on the patient’s history of malignant melanoma with disseminated metastatic disease, it was felt that the ileal lesion responsible for the intussusception represented a new metastatic deposit. Given the intermittently symptomatic nature of the intussusception, the patient underwent a laparoscopic small bowel resection. On laparoscopy, an ileoileal intussusception was noted 20 cm proximal from the ileocecal valve (Figure 2). The involved segment of ileum was resected, and a stapled side-to-side anastomosis was made. Macroscopic examination of the resected specimen revealed a 50 mm segment of telescoping of the bowel with a 30 mm polypoid lesion at the lead point. Microscopically, the tumor nodule was composed of sheets of malignant cells of epithelioid type with large pleomorphic nuclei, prominent nucleolus, and moderately abundant cytoplasm (Figure 3A). The tumor cells showed positive staining for S100, SOX 10, and vimentin, consistent with metastatic melanoma (Figure 3B).
Postoperatively, the patient made a good recovery, and was discharged from the hospital four days following surgery. The patient was followed up in the surgical outpatient clinic four weeks postoperatively, and he was recovering well with complete resolution of his abdominal symptoms. He was subsequently restarted on his immunotherapy.
DISCUSSION
Adult intussusception is less common in frequency and also differs in clinical presentation when compared with intussusception in children. Pediatric patients with intussusception classically present with a triad of acute abdominal pain, a palpable sausage-shaped abdominal mass, and currant-jelly stools. In contrast, clinical presentation of adults with intussusception tends to be more variable, and is often subacute or chronic in nature. In one case series of 41 adults with intussusception, the duration of symptoms varied from six hours to three years, and 75.6% of cases presented with subacute or chronic symptoms [7]. Symptoms may include abdominal pain, nausea and/or vomiting, bloody stools, changes in bowel habits, and presence of abdominal mass.
Commonly utilized imaging modalities for evaluation of intussusception include ultrasound (US) and CT. Typical US findings of intussusception include the target sign on the transverse view, and the pseudokidney sign on the longitudinal view [8],[9]. On CT, a pathognomonic finding for intussusception is the presence of a bowel-within-bowel configuration with or without mesenteric fat and mesenteric vessels [6]. This configuration can be described as a target sign when the CT images are perpendicular to the longitudinal axis of the intussusception, or as a sausage sign when the images are parallel to the longitudinal axis [10].
Intussusception can be classified according to the location of the lead point as follows in order of decreasing frequency: enteric (entero-enteric), colo-colonic, ileocolic, sigmoido-rectal, and recto-rectal [1],[3],[7]. Intussusception can also be classified on the basis of etiology, and can initially be divided into two groups: intussusception without a lead point lesion (i.e., primary or idiopathic intussusception), and intussusception with a lead point (i.e., secondary intussusception). Intussusception without a lead point lesion, which accounts for about 10% of intussusception in adults [11], is most frequently discovered incidentally in patients without any underlying pathology, although there are such cases that have been reported in patients with celiac disease and Crohn’s disease [12],[13]. These cases are more likely to be transient and self-limited, compared to intussusception caused by a lead point lesion, which tends to be persistent or recurrent [6]. Intussusception with a lead point, which accounts for about 90% of cases in adults, is due to an underlying pathological lesion. The lesions can be benign in nature, such as lipoma, adenomatous polyp, and Meckel’s diverticulum, or they can be malignant, which can be a primary bowel malignancy, a metastatic lesion, or lymphoma. Intussusception in the colon is more likely to be due to a malignant lesion compared to that in the small bowel, as malignancy accounts for between 40 and 63% of adult intussusception in the colon, compared to between 14 and 29% of cases in the small intestine [14],[15],[16]. Computed tomography features of intussusception associated with a pathological lead point include presence of a mass at the lead point, radiological bowel obstruction, and longer length and larger diameter of the intussusception when compared to one without a lead point [6],[17],[18]. In addition, older age (especially if greater than 60 years) or a known history of malignancy should alert the treating clinician of a possible malignant etiology [19].
When managing adult intussusception, it is important to first identify clinical or radiological signs of obstruction, bowel ischemia, or perforation. If present, emergent surgical exploration should be undertaken, which may be performed via laparoscopy or laparotomy depending on patient factors and surgeon expertise.
In cases of small bowel intussusception without obstruction, ischemia or perforation, patient’s demographics, medical history, clinical and radiological features should be reviewed to assess the likelihood of a pathological lead point. Patients, who are older than 60 years of age, have a history of malignancy, or presenting with persistent or recurrent intussusception with CT findings suggestive of a pathological lead point should be surgically explored with a view to perform a bowel resection for definitive diagnosis and management. In younger patients presenting with small bowel intussusception without suspicious clinical or radiological features, the possibility of intussusception without a pathological lead point should be considered. In such cases, one management option is to perform a diagnostic laparoscopy, and if intussusception is present at the time of operation, a resection should be performed for definitive diagnosis [19]. An alternative etiology may be evident during laparoscopy, such as a Meckel’s diverticulum or adhesions, which can be managed accordingly. A negative laparoscopy with no intussusception present at operation and with no obvious pathology suggests a transient intussusception without a pathological lead point, and this can be managed without a resection. Another management option in patients with a low probability of a pathological lesion is nonoperative management. There are cases reported in the literature where conservative management was successfully utilized [20], but caution needs to be exercised with this approach as it is possible to miss a pathological lead point which was not readily identified on initial imaging. These cases should therefore be followed up with follow up imaging and endoscopic evaluation.
Colonic intussusception, on the other hand, is more likely to be caused by a malignant lead point. The standard treatment is surgical resection of the affected colonic segment using oncological surgical principles. Colonoscopy may be considered preoperatively for direct visualization and histological assessment by performing a biopsy [7],[21]. Controversy exists as to whether an endoscopic or laparoscopic reduction should be attempted prior to resection. Proponents argue that preoperative reduction may allow for a more limited resection [22]. For example, a case reported by Tatarian et al. [23] describes a patient who presented with a colorectal intussusception due to an invasive adenocarcinoma at the rectosigmoid junction who was initially managed with endoscopic reduction followed by sigmoid colectomy. Here the authors felt that without a reduction, the patient would have been unable to have a sphincter-preserving surgery and would have required an abdominoperineal resection. However, preoperative reduction is generally not recommended and should be exercised with caution, as there is a risk of perforation during manipulation, as well as the theoretical risk of tumor spillage and seeding [1],[24].
In our case, the entero-enteric intussusception was caused by a metastatic deposit of malignant melanoma. Malignant melanoma is the most common metastatic lesion of the small or large intestine [25]. Patients with gastrointestinal metastases from melanoma can present with abdominal pain, nausea or vomiting, obstruction, intussusception, or with gastrointestinal (GI) bleeding. Surgery is traditionally reserved for patients who are symptomatic, however, there are reports demonstrating increased median survival in patients who underwent surgical excision for abdominal metastases of malignant melanoma (especially if complete abdominal tumor extirpation was achieved) compared to those who were treated medically [25],[26].
CONCLUSION
Intussusception in adults is rare, and is often associated with a pathological lead point. Patients with older age, known history of malignancy, CT findings suggestive of a malignant lead point, and colonic intussusception are more likely to have a malignant lead point. A low threshold for surgical exploration is recommended for definitive diagnosis of the cause.
REFERENCE
1.
Zubaidi A, Al-Saif F, Silverman R. Adult intussusception: A retrospective review. Dis Colon Rectum 2006;49(10):1546–51. [CrossRef]
[Pubmed]

2.
Azar T, Berger DL. Adult intussusception. Ann Surg 1997;226(2):134–8. [CrossRef]
[Pubmed]

3.
Weilbaecher D, Bolin JA, Hearn D, Ogden W 2nd. Intussusception in adults. Review of 160 cases. Am J Surg 1971;121(5):531–5. [CrossRef]
[Pubmed]

4.
Carter CR, Morton AL. Adult intussusception in Glasgow, UK. Br J Surg 1989;76(7):727. [CrossRef]
[Pubmed]

5.
Yalamarthi S, Smith RC. Adult intussusception: Case reports and review of literature. Postgrad Med J 2005;81(953):174–7. [CrossRef]
[Pubmed]

6.
Kim YH, Blake MA, Harisinghani MG, et al. Adult intestinal intussusception: CT appearances and identification of a causative lead point. Radiographics 2006;26(3):733–44. [CrossRef]
[Pubmed]

7.
Wang N, Cui XY, Liu Y, et al. Adult intussusception: A retrospective review of 41 cases. World J Gastroenterol 2009;15(26):3303–8. [CrossRef]
[Pubmed]

8.
Weissberg DL, Scheible W, Leopold GR. Ultrasonographic appearance of adult intussusception. Radiology 1977;124(3):791–2. [CrossRef]
[Pubmed]

9.
Boyle MJ, Arkell LJ, Williams JT. Ultrasonic diagnosis of adult intussusception. Am J Gastroenterol 1993;88(4):617–8.
[Pubmed]

10.
Gayer G, Zissin R, Apter S, Papa M, Hertz M. Pictorial review: Adult intussusception—a CT diagnosis. Br J Radiol 2002;75(890):185–90. [CrossRef]
[Pubmed]

11.
Haas EM, Etter EL, Ellis S, Taylor TV. Adult intussusception. Am J Surg 2003;186(1):75–6. [CrossRef]
[Pubmed]

12.
Agha FP. Intussusception in adults. AJR Am J Roentgenol 1986;146(3):527–31. [CrossRef]
[Pubmed]

13.
Knowles MC, Fishman EK, Kuhlman JE, Bayless TM. Transient intussusception in Crohn disease: CT evaluation. Radiology 1989;170(3 Pt 1):814. [CrossRef]
[Pubmed]

14.
Felix EL, Cohen MH, Bernstein AD, Schwartz JH. Adult intussusception; case report of recurrent intussusception and review of the literature. Am J Surg 1976;131(6):758–61. [CrossRef]
[Pubmed]

15.
Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg 1997;173(2):88–94. [CrossRef]
[Pubmed]

16.
Nagorney MD, Sarr MG, McIlrath CD. Surgical management of intussusception in the adult. Ann Surg 1981;193(2):230–6. [CrossRef]
[Pubmed]

17.
Lvoff N, Breiman RS, Coakley FV, Lu Y, Warren RS. Distinguishing features of self-limiting adult small-bowel intussusception identified at CT. Radiology 2003;227(1):68–72. [CrossRef]
[Pubmed]

18.
Rea JD, Lockhart ME, Yarbrough DE, Leeth RR, Bledsoe SE, Clements RH. Approach to management of intussusception in adults: A new paradigm in the computed tomography era. Am Surg 2007;73(11):1098–105.
[Pubmed]

19.
Varban OA, Ardestani A, Azagury DE, Kis B, Brooks DC, Tavakkoli A. Contemporary management of adult intussusception: Who needs a resection? World J Surg 2013;37(8):1872–7. [CrossRef]
[Pubmed]

20.
Aydin N, Roth A, Misra S. Surgical versus conservative management of adult intussusception: Case series and review. Int J Surg Case Rep 2016;20:142–6. [CrossRef]
[Pubmed]

21.
M'rabet S, Jarrar MS, Akkari I, et al. Colonic intussusception caused by a sigmoidal lipoma: A case report. Int J Surg Case Rep 2018;50:1–4. [CrossRef]
[Pubmed]

22.
Barussaud M, Regenet N, Briennon X, et al. Clinical spectrum and surgical approach of adult intussusceptions: A multicentric study. Int J Colorectal Dis 2006;21(8):834–9. [CrossRef]
[Pubmed]

23.
Tatarian T, Arkonac D, Phillips B, Isenberg GA, Goldstein SD. Colonic adenocarcinoma presenting as sigmoidorectal intussusception: A consideration for intussusception reduction. Am Surg 2016;82(8):e181–2.
[Pubmed]

24.
Dungerwalla M, Loh S, Smart P. Adult colonic intussusception: Surgery still the best option. J Surg Case Rep 2012;2012(6):3. [CrossRef]
[Pubmed]

25.
Branum GD, Seigler HF. Role of surgical intervention in the management of intestinal metastases from malignant melanoma. Am J Surg 1991;162(5):428–31. [CrossRef]
[Pubmed]

26.
Gutman H, Hess KR, Kokotsakis JA, Ross MI, Guinee VF, Balch CM. Surgery for abdominal metastases of cutaneous melanoma. World J Surg 2001;25(6):750–8. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Ho Nam Choi - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Yasser Arafat - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Iman Antoun - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2019 Ho Nam Choi et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.