|
Case Report
Fatal arrhythmias despite early recognized successful treatment of digoxin toxicity
1 DO, Internal Medicine Chief Resident, MercyOne North Iowa Internal Medicine Residency, Mason City, Iowa, USA
2 Third Year Osteopathic Medical Student (OMS3), Des Moines University College of Osteopathic Medicine, Des Moines, Iowa, USA
3 MD, Internal Medicine Faculty Attending, MercyOne North Iowa Internal Medicine Residency, Mason City, Iowa, USA
Address correspondence to:
Babajide Adio
DO, 1000 4th St SW, Mason City, Iowa 50401,
USA
Message to Corresponding Author
Article ID: 100080Z06BA2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Adio B, Strandlund SJ, Delaney TP. Fatal arrhythmias despite early recognized successful treatment of digoxin toxicity. Case Rep Int 2020;9:100080Z06BA2020.ABSTRACT
Introduction: Digoxin is used to treat severe systolic heart failure and atrial fibrillation. Due to its narrow therapeutic window, toxicity has been well documented. Prompt treatment with the reversal agent, Digoxin Immune Fab is required in cases of digoxin toxicity to decrease mortality. However, little is known regarding the sequela following immediate successful reversal of toxicity. We report the case of a patient who developed potentially fatal ventricular arrhythmias following early recognized successful treatment of digoxin toxicity with Digoxin Immune Fab.
Case Report: We report a case of a 69-year-old man with a history of systolic heart failure and atrial fibrillation who presented with altered mental status and gait instability. Polypharmacy was first considered; hence his medications were discontinued, or dose adjusted. Normal pressure hydrocephalus was another diagnosis considered. However, when laboratory data revealed elevated potassium of 5.2 mmol/L, acute kidney injury, elevated serum digitalis at 2.6 ng/mL, prompt diagnosis of digoxin toxicity was made. Digoxin Immune Fab was administered with immediate improvement of patient’s symptoms and labs. However, he experienced runs of ventricular tachycardia and supraventricular tachycardia with aberrancy in the days following. The patient then had further cardiac work-up requiring transfer to a tertiary care center for an ablation procedure.
Conclusion: While arrhythmias associated with digoxin toxicity have been well documented, little is known of delayed arrhythmias following the use of a reversal agent. We report a rare case of potentially fatal delayed ventricular arrhythmias after early recognized successful treatment of digoxin toxicity with Digoxin Immune Fab.
Keywords: Digoxin Immune Fab, Digoxin toxicity, Hyperkalemia, Ventricular arrhythmias
INTRODUCTION
Digoxin is one of the oldest cardiac medications still in use today. It is used to treat severe cases of systolic heart failure and atrial fibrillation due to its potent inotropic and electrochemical effects on cardiac tissue [1]. Digoxin has a narrow therapeutic window, which is a serum digoxin concentration between 1 and 2.6 nmol/L for normal individuals. Evidence shows patients with congestive heart failure have better outcomes at a concentration of 0.5–0.9 nmol/L [1]. Due to this narrow therapeutic window and the potentially lethal effects of toxicity, this medication is not first line. While it has been shown to decrease hospitalizations in heart failure patients, it has also been shown to worsen mortality [2]. The effects of toxicity include acute kidney injury, hyperkalemia, arrhythmias, and neurological effects including generalized weakness, drowsiness, vision changes, and confusion [1],[3]. Death can occur due to ventricular fibrillation or ventricular tachycardia. There should be a high index of suspicion in patients taking digoxin who present with any of the above symptoms so that early treatment can be initiated. While much is known about mortality associated with digoxin toxicity, little is known of the sequela after prompt and successful treatment with Digoxin Immune Fab. We report a case of a patient who presented with symptoms of digoxin toxicity that resolved with Digoxin Immune Fab treatment, however continued to experience numerous runs of ventricular arrhythmias in the days following.
CASE REPORT
A 69-year-old man presented to the emergency department (ED) with altered mental status, decreased urine output, and gait instability resulting in numerous falls over the past few days. His family provided most of the history. They reported that the patient had been confused, fallen multiple times, and urinated once over the last few days.
The patient’s medical history included heart failure with reduced ejection fraction (HFrEF) of 25% status post-biventricular automatic implantable cardioverter defibrillator (AICD), atrial fibrillation, coronary artery disease, right hip osteoarthritis, chronic low back pain, non-insulin-dependent diabetes, benign prostatic hyperplasia, and depression. He was taking numerous prescribed medications including but not limited to amiodarone 200 mg daily, mexiletine 200 mg twice a day, digoxin 125 mcg daily, aripiprazole 10 mg daily, finasteride 5 mg daily, gabapentin 400 mg daily, atorvastatin 40 mg daily, duloxetine 30 mg daily, metformin 500 mg twice a day, metoprolol succinate 100 mg daily, morphine extended release 60 mg twice a day, risperidone 1 mg daily, lamotrigine 200 mg daily, and dabigatran 150 mg twice a day.
On physical exam, the patient was confused. Lungs were clear to auscultation. Cardiac and abdominal exams were unremarkable. Initial vital signs in the ED were significant for a pulse of 65 beats per minute, respiratory rate of 20 breaths per minute, and oxygen saturation of 87% on 2 liters supplemental oxygen. His systolic blood pressure (SBP) dropped to the 60s to 80s mmHg with diastolic pressure (DBP) of 40s to 50s mmHg. He was given a liter of normal saline and supplemental oxygen was increased to 3 liters. He was then transferred to the critical care unit (CCU) for close observation and further evaluation.
Initial laboratory findings showed unremarkable cardiac biomarkers. Creatinine showed a significant increase of 4.26 mg/dL compared to his base line of 1–1.2 mg/dL. Basic metabolic panel showed an initial potassium level of 4.8 mmol/L. Overnight, the patient required more fluids to keep systolic blood pressure over 90 mmHg. The next morning, creatinine was reduced to 3.22 mg/dL, potassium was now elevated at 5.2 mmol/L, and serum digitalis was elevated at 2.6 ng/mL while remembering that patients with congestive heart failure have better outcomes at serum digitalis concentration of 0.5–0.9 ng/mL (Table 1). Blood and urine cultures showed no growth.
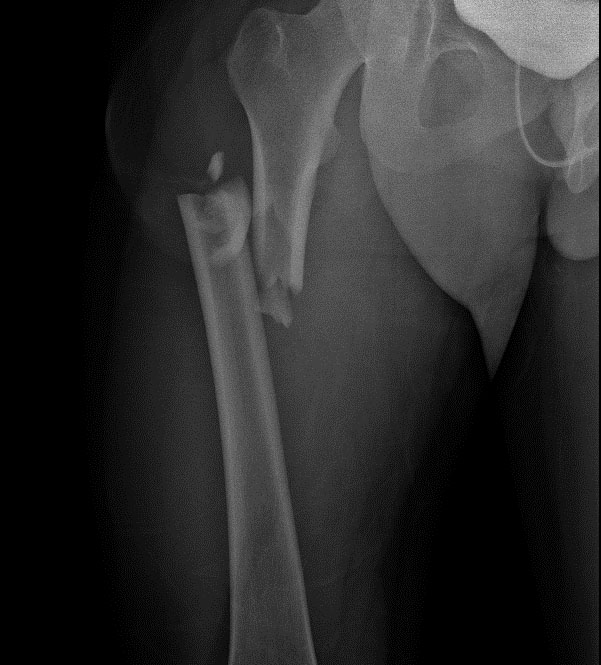
Imaging included renal ultrasound that revealed no obvious signs of obstruction. A head computed tomography (CT) without contrast showed ventriculomegaly slightly out of proportion to the amount of atrophy combined with mild crowding of the sulci and gyri suggesting possible normal pressure hydrocephalus. An electrocardiogram (EKG) did not show the classic signs of digoxin toxicity; however, it was difficult to interpret considering his AICD (Figure 1). A transthoracic echocardiogram showed reduced ejection fraction of 25%, unchanged from a month prior.
Polypharmacy and normal pressure hydrocephalus were considered as initial differential diagnoses. Due to the patient’s elevated creatinine and decreased urine output, acute kidney injury was also high on that differential. Upon reviewing his medication list, his metformin and morphine were discontinued immediately on admission. His other medications including gabapentin, lamotrigine, dabigatran, risperidone, duloxetine, and metoprolol succinate were all decreased. We were also concerned that his normal pressure hydrocephalus could have worsened. Ventriculomegaly was seen on previous head CT from five months and one month earlier without any convincing evidence of normal pressure hydrocephalus. However, no lumbar puncture had been done for a definitive diagnosis of normal pressure hydrocephalus. He was scheduled to follow up with neurology as an outpatient but had not yet done so. Once the serum digitalis level was obtained, we quickly narrowed our differential to digoxin toxicity especially in the setting of his hyperkalemia, altered mental status, and acute kidney injury. Digoxin was subsequently discontinued from his medication list and Digoxin Immune Fab was ordered.
Dosage is calculated by multiplying serum digoxin concentration (ng/mL) by patient weight (kg) divided by 100. In this case, the calculation was 2.6*100/100, roughly 2.6 vials (4 mL per vial). It is recommended to round up to the next full vial. However, we decided to give two vials of Digoxin Immune Fab to the patient in the CCU. This decision was made based on the patient’s improvement in creatine from 4.26 ng/dL on admission to 3.8 ng/dL the next morning after fluid administration and medication changes. The patient’s symptoms and acute kidney injury appeared to be gradually improving, suggesting an improvement in digitalis toxicity, and it was decided to start with just two vials of Digoxin Immune Fab. Potassium was measured every four hours post Digoxin Immune Fab. Potassium quickly dropped from 5.2 to 4.1 mmol/L and remained consistent around 4.1 mmol/L until discharge. Six hours following Digoxin Immune Fab administration, the patient’s confusion and oliguria remarkably improved. Follow-up serum digitalis level was 1.9 ng/mL the next morning and he was able to be transferred to the general medicine floor (Table 1).
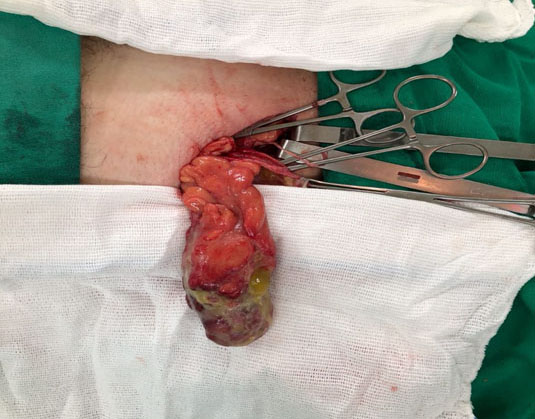
After resolution of his initial symptoms of digoxin toxicity, a plan was made to discharge the patient to a skilled facility for physical therapy. However, on the morning of planned discharge, he had few runs of non-sustained ventricular tachycardia resulting in his AICD firing twice (Figure 2). So discharge was postponed. He continued to have a few runs of non-sustained ventricular tachycardia and supraventricular tachycardia with aberrancy causing his AICD to continue to fire again the next day. Cardiology was consulted and the patient was transferred to the cardiac floor and started on amiodarone drip in addition to his current medication regime, which included amiodarone 200 mg daily and mexiletine 200 mg twice a day. The patient had a history of three prior cardiac catheterizations in the last 15 years, most recently a year prior showing non-occlusive disease with EF of 25%. Another ischemic work-up was done with cardiac catheterization which still showed minimal non-occlusive coronary artery disease but showed a significantly decreased ejection fraction of 10%, down from 25% noted on transthoracic echocardiogram a week prior. The patient was then transferred to a tertiary care center where he underwent an ablation for supraventricular tachycardia and did well afterwards.
DISCUSSION
Digoxin is primarily eliminated by the kidneys and can build up in the body with any type of renal impairment. It also has a narrow therapeutic window, and symptoms of toxicity can be seen with serum digitalis levels over 2.0 ng/mL. However, in patients with heart failure the goal range of serum digitalis has been reduced to 0.5–0.9 ng/mL [3]. Our patient had a long history of systolic heart failure with other comorbidities and presented with a serum digitalis level of 2.6 ng/mL. However, while his serum digitalis level was elevated, his numerous signs and symptoms including confusion, depth perception difficulties, weakness, and gait problems predisposing him to falls were the most important diagnostic indicator of digitalis toxicity. A diagnosis of digoxin toxicity was made based on high clinical suspicion due to the presence of signs and symptoms of toxicity as well as his acute kidney injury with oliguria, hyperkalemia, and elevated serum digitalis level.
Digoxin can be used in the treatment of atrial fibrillation or systolic heart failure. However, its use has declined since the 1990s due to the introduction of newer drugs and digoxin’s risk of toxicity [3]. It is now reserved for cases refractory to first line treatment of systolic heart failure. Digoxin works by inhibiting the sodium–potassium pump, increasing intracellular calcium in cardiac myocytes. This action increases contractility of the heart but also causes systemic hyperkalemia [4]. This electrolyte imbalance places the patient at risk for cardiac arrhythmias, a serious complication of digoxin toxicity. A previous study was done looking at mortality associated with serum potassium levels in patients taking rate and rhythm control medication, of which 49% of patients were taking digoxin [5]. They found that the highest mortality rate was in patients with serum potassium >5.0 mmol/L, resulting in 20% of cases of mortality. Of all the rhythm and rate controlling drugs, digoxin conferred the highest increased mortality risk associated with both hyperkalemia (>5.0 mmol/L) and hypokalemia (<3.5mmol/L), with a nearly two-fold increase in 90-day all-cause mortality risk [5]. This was a key factor in our treatment decision because our patient had potassium of 5.2 mmol/L. It was important to get serum potassium under 5.0 mmol/L in order to decrease his mortality risk. This was achieved with emergent reversal of digoxin with Digoxin Immune Fab.
Digoxin Immune Fab is used to treat digoxin toxicity. It binds digoxin forming a complex that is excreted in the urine. Indications for its use include arrhythmias, cardiac arrest, or hyperkalemia [6],[7].
While Digoxin Immune Fab is a relatively benign medication, it still carries risk of side effects such as exacerbation of heart failure, increased ventricular rates, and hypokalemia that are uncommon but can occur, especially in patients with multiple comorbidities [6],[8]. This may be a result of “rebound toxicity” that can occur following a rapid correction of serum digitalis and results in up to 2% of patients who receive Digoxin Immune Fab. This can develop as quickly as 24 hours after administration, but up to 10 days later in patients with renal disease [3]. Our patient had a long list of comorbidities including HFrEF and renal impairment, so it is reasonable to consider that the use of Digoxin Immune Fab exacerbated his already failing heart and triggered the arrhythmias that appeared in the days following. The other main side effect of Digoxin Immune Fab is increased ventricular rates, which also may have contributed to the numerous runs of ventricular tachycardia and supraventricular tachycardia that the patient experienced following treatment. It is important to consider that the reversal agent is a medication itself and thus can have side effects. Our patient only received two vials of Digoxin Immune Fab even though standard convention would have been three vials. The patient therefore received a lower dose of Digoxin Immune Fab to treat his specific serum digitalis level. While medications can have side effects at any dose, we believe it was less likely in this situation but still cannot be ruled out.
It is also important to consider other potential causes of the arrhythmias which our patient experienced in the days following reversal. For example, the arrhythmias may have been due to a physiological effect following the relatively rapid decrease in serum digoxin due to the correct working of Digoxin Immune Fab, like the “rebound toxicity” effect mentioned earlier. In this case, the patient had been on digoxin for years and it is reasonable to consider that a relatively rapid decrease in serum levels could put him at risk for arrhythmias, especially considering his comorbidities. Another cause of the arrhythmias could have been due to an unknown sequela or late complication of digoxin toxicity because arrhythmias are one of the many known complications which can occur with toxicity. Although recognition of the toxicity and administration of the reversal agent were done quickly leading to improvement of the patient’s presenting symptoms, this could still be a possibility.
Overall, it is important to note that Digoxin Immune Fab does not come without risks. In this case, the arrhythmias that our patient experienced could have been due to the side effects of the reversal agent itself, a sequela of digoxin toxicity, or it may have been the medication working correctly, leading to the relatively rapid decrease in serum digitalis that triggered those events.
CONCLUSION
Upon literature review, there have been many cases of arrhythmias associated with digoxin toxicity. However, to the best of our knowledge, there has not been any reported cases of delayed ventricular arrhythmias following treatment of digoxin toxicity. We report the first case of a patient with acute digoxin toxicity treated emergently with Digoxin Immune Fab but who subsequently developed potentially fatal ventricular arrhythmias. Better understanding of the effects of digoxin toxicity following early successful treatment may prevent the development of potentially fatal arrhythmias.
REFERENCE
1.
MacLeod-Glover N, Mink M, Yarema M, Chuang R. Digoxin toxicity: Case for retiring its use in elderly patients? Can Fam Physician 2016;62(3):223–8.
[Pubmed]

2.
Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. New Engl J Med 1997;336(8):525–33. [CrossRef]
[Pubmed]

3.
Pincus M. Management of digoxin toxicity. Aust Prescr 2016;39(1):18–20. [CrossRef]
[Pubmed]

4.
Saad AF, Monsivais L, Pacheco LD. Digoxin therapy of fetal superior ventricular tachycardia: Are digoxin serum levels reliable? AJP Rep 2016;6(3):e272–6. [CrossRef]
[Pubmed]

5.
Hagengard L, Søgaard P, Espersen M, et al. Association between serum potassium levels and short-term mortality in patients with atrial fibrillation or flutter co-treated with diuretics and rate- or rhythm-controlling drugs. Eur Heart J Cardiovasc Pharmacother 2019. pii: pvz024. [CrossRef]
[Pubmed]

6.
Chan BS, Buckley NA. Digoxin-specific antibody fragments in the treatment of digoxin toxicity. Clin Toxicol (Phila) 2014;52(8):824–36. [CrossRef]
[Pubmed]

7.
Hauptman PJ, Blume SW, Lewis EF, Ward S. Digoxin toxicity and use of digoxin immune fab: Insights from a national hospital database. JACC Heart Fail 2016;4(5):357–64. [CrossRef]
[Pubmed]

8.
Janssen RM, Berg M, Ovakim DH. Two cases of cardiac glycoside poisoning from accidental foxglove ingestion. CMAJ 2016;188(10):747–50. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Babajide Adio - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Sara J Strandlund - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Thomas P Delaney - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Babajide Adio et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.