|
Case Report
Methylene blue in the management of severe distributive shock in calcium channel blocker overdose
1 Resident Medical Officer, Anaesthetics Department, Joondalup Health Campus, Perth, Western Australia, Australia
2 CICM, Consultant Intensive Care, Joondalup Health Campus, Perth, Western Australia, Australia
Address correspondence to:
Annica Bester
Joondalup Health Campus, Shenton Ave, Joondalup, Western Australia 6027,
Australia
Message to Corresponding Author
Article ID: 100082Z06AB2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Bester A, Roeck MA. Methylene blue in the management of severe distributive shock in calcium channel blocker overdose. Case Rep Int 2020;9:100082Z06AB2020.ABSTRACT
Introduction: Deliberate polypharmacy overdose is associated with an increasing proportion of admissions to the intensive care unit. Overdose on hemodynamic active substances such as calcium channel blockers can be fatal as it is associated with severe distributive shock. Methylene blue has drawn attention in critical care medicine for its use in the management of distributive shock, particularly in cases of anaphylaxis, septic shock, and shock following cardiac bypass surgery. We describe the use of methylene blue in the management of refractory shock due to calcium channel blocker (CCB) overdose.
Case Report: We present a case of benzothiazepine type CCB overdose which leads to admission to the intensive care unit for the management of severe distributive shock. Conventional treatments including vasopressors and high dose insulin therapy were instituted, but despite these treatments the patient remained hypotensive. The decision was made to administer methylene blue following which the patient achieved hemodynamic stability and was successfully weaned off all vasopressors.
Conclusion: This case report specifically focuses on the use of methylene blue in distributive shock secondary to CCB overdose. Currently there are no randomized control trials to support its use, and evidence is limited to observational studies including single case reports. In this case report we describe the mechanism of action of methylene blue and why we believe it makes for the perfect adjunct therapy in calcium channel blocker overdose.
Keywords: Calcium channel blocker overdose, Distributive shock, Methylene blue, Refractory shock
INTRODUCTION
Polypharmacy overdose accounts for an increase in proportion of intensive care unit (ICU) admissions and is associated with a high morbidity and mortality [1],[2]. Overdose on hemodynamic active substances such as calcium channel blocker (CCB) medications can be fatal as it is associated with severe distributive shock, characterized by a reduction in peripheral vascular resistance and an increase in cardiac output [3],[4].
To our knowledge, there are no randomized controlled human trials to evaluate different treatment methods for the management of CCB overdose. Conventional treatment modalities for CCB overdose include intravenous (IV) fluids and calcium, vasopressors, and high dose insulin therapy [5].
We suggest the use of methylene blue in the use of distributive shock secondary to CCB overdose as an adjunct treatment to conventional therapies. Methylene blue has been described in literature for its use in distributive shock in anaphylaxis, sepsis, and cardiac bypass surgery [6],[7],[8],[9]. It acts by inhibiting guanylate cyclase, leading to a reduction in cyclic guanosine monophosphate (cGMP) and thus reducing vascular smooth muscle relaxation [7],[8]. Methylene blue also reduces the production of nitrous oxide, by directly inhibiting nitrous oxide synthase [7],[8]. The mechanism of action of methylene blue makes it the ideal drug that directly counteracts the effects that CCB medications have on smooth muscle.
We present a case benzothiazepine type CCB overdose which leads to admission to the ICU for the management of severe distributive shock. Conventional treatments including IV calcium, vasopressors, and high dose insulin therapy were instituted, but despite these treatments the patient remained in shock. The decision was made to administer methylene blue, following which the patient achieved hemodynamic stability and was successfully weaned off all vasopressors.
CASE REPORT
A 49-year-old Caucasian female with a past medical history of post-traumatic stress disorder, depression, and ischemic heart disease was brought in by ambulance following polypharmacy overdose. The patient took a total of 10800 mg diltiazem SR capsules, 280 mg citalopram, 100 mg rosuvastatin, and 125 mg doxylamine tablets at 1:00 am. Following multiple episodes of vomiting at home, the patient told her partner about the overdose at 9:00 am, after which her partner proceeded to call an ambulance.
The patient was brought to the emergency department at 9:45 am. On arrival, the patient was alert and able to maintain her own airway, respiratory rate of 20 breaths per minute, oxygen saturations 96% on room air, blood pressure (BP) 90/52 mmHg, heart rate (HR) 78 beats per minute, and no recorded fever. The patient was warm, well perfused with strong peripheral pulses. Systems examination was otherwise unremarkable. The patient was very restless and agitated at the time and reported feeling nauseous.
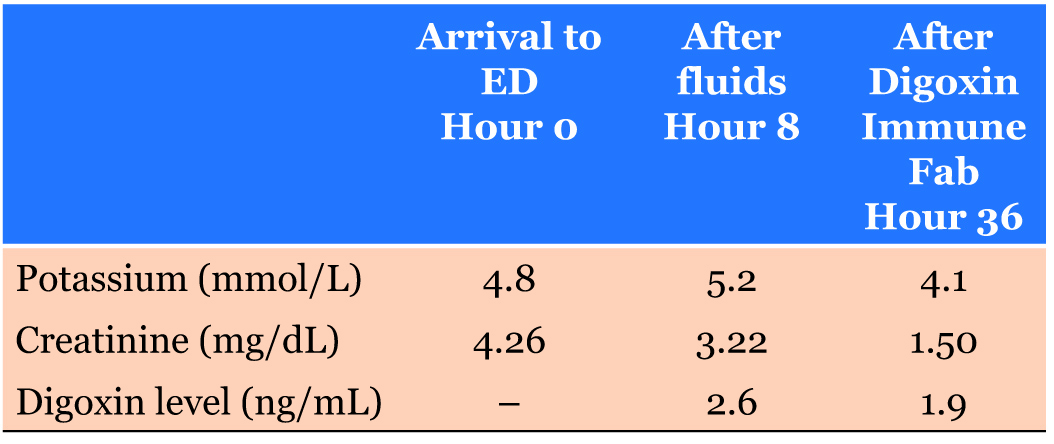
Investigations
Laboratory studies at presentation included a complete blood count, renal function and electrolytes, paracetamol and blood alcohol levels, which were largely unremarkable. A venous blood gas revealed a pH of 7.29 and a lactate of 7.1. Electrocardiogram (ECG) showed ST depression in lead V3 and V4. Bedside echo was performed by the intensivist and showed a preserved left ventricular ejection fraction, with a cardiac output of 7 L/min and stroke volume of 80 mL as measured by FloTrac monitor. Chest X-ray revealed diffuse infiltrates throughout the lung fields with more focal consolidation in the left mid to lower zone.
Working Diagnosis
The working diagnosis at the time was distributive shock. Although it was a polypharmacy overdose, the main mechanism of shock was thought to be mediated by the CCB as this was taken in large quantity. Given the history of vomiting and the findings on the chest X-ray, sepsis secondary to aspiration pneumonia was considered as a potential contributor to distributive shock.
Management
Initial management in the emergency department included IV fluid resuscitation with 1 L normal saline given stat and repeated 1 hour later. Central and arterial access was achieved promptly and an indwelling catheter was inserted. Electrolytes were optimized with IV replacements, including IV calcium gluconate. Blood pressure 1 hour following fluid resuscitation was 98/50 mmHg and 3 hours later 82/45 mmHg and the decision was made to commence hemodynamic support with a norepinephrine infusion. The patient was also commenced on an insulin and dextrose infusion, with an initial bolus of 1 unit/kg and continued at a rate of 0.5 unit/kg/hour (titrated to 1 unit/kg/hour). The on-call toxicologist was contacted and agreed with the management instituted and advised against lipid emulsion therapy.
The patient was admitted to the ICU for hemodynamic support. At 6:30 pm the mental state of the patient deteriorated in the ICU. The decision was made to intubate the patient for airway protection due to reduced Glasgow coma scale, following a vomiting episode and anticipating further cardiovascular instability. Additional treatments included 3 boluses of insulin and dextrose (two at 2 units/kg and one at 1 unit/kg boluses), while continuing infusion rate at 1 mL/kg/hour, 8 mg IV hydrocortisone and bowel irrigation via administration of continuous PicoPrep (sodium picosulfate, magnesium oxide, and citric acid combination) via the nasogastric tube. The patient was empirically started on IV piperacillin/tazobactam to treat for suspected aspiration. Electrolytes were monitored by arterial blood gases and formal laboratory electrolytes and renal function. Potassium and magnesium were replaced as needed.
Despite the treatments instituted, the patient continued to require escalating doses of norepinephrine and vasopressin infusions. High dose insulin was continued but after 4 hours the patient was still significantly hypotensive. After exclusion of contraindications the decision was made to administer methylene blue at 1.5 mg/kg as an infusion over 30 minutes.
Outcome
Prior to methylene blue administration, escalating doses of vasopressors were required to maintain a target mean arterial pressure (MAP) of 65 mmHg. Within 1 and 6 hours of methylene blue administration, norepinephrine and vasopressin requirements remained stable. Within 24 hours of methylene blue administration, norepinephrine requirements reduced by 50% and vasopressin requirement remained stable for the target MAP of 65 mmHg, and insulin therapy was weaned off. The patient was completely weaned off hemodynamic support day 5 of admission and MAP remained stable at or greater than 65 mmHg. After 5 days, the patient was extubated and following inpatient psychiatric review was transferred to the psychiatric inpatient facility for further management.
DISCUSSION
Calcium channel blocker medications can produce profound hypotension when taken in large quantities [3]. The type of shock produced is usually a distributive shock due to reduction in systemic vascular resistance and often accompanied by an increase in cardiac output [9]. When taking in large quantities, diltiazem can cause profound hypotension as well as bradycardia due to its negative ionotropic and chronotropic effects [4],[9],[10]. Our patient was not observed to be bradycardic, but presented with shock with a distributive picture.
Current expert consensus on the recommended treatment modalities for CCB overdose include IV calcium, high dose insulin therapy, and vasopressors in the presence of shock [5]. These treatments can be instituted alone or in combination [5]. For patients in refractory shock failing to respond to first-line treatment, the suggested treatments include incremental doses of high dose insulin therapy in the presence of myocardial dysfunction (level 1D evidence) or without evidence of myocardial dysfunction (level 2D evidence), IV lipid emulsion therapy (level 1D evidence), pacemakers if bradycardia is present (level 2D evidence), and venoarterial extracorporeal membrane oxygenation (VAECMO) in the presence of cardiogenic shock (level 2D evidence) [5]. However, many of these treatments are supported by limited number of case series and only level 2 evidence (relatively weak).
Our patient was failing the recommended conventional treatment modalities of IV calcium, vasopressors and high dose insulin therapy, and was in refractory shock. We decided to institute the treatment of methylene blue as an adjunct therapy. The mechanism of action of methylene blue makes it the ideal drug that directly counteracts the effects that calcium channel blockers have on smooth muscle. Calcium channel blockade prevents the influx of calcium into cells, which subsequently reduces the amount of calcium within the cells leading to smooth muscle relaxation [3]. Methylene blue acts by inhibiting guanylate cyclase, leading to a reduction in cGMP and thus increases intracellular calcium and increases vascular smooth muscle contraction [7],[8] (Figure 1). Methylene blue also reduces the production of nitrous oxide (NO), by directly inhibiting NO synthase [7],[8]. Together, these actions counteract the effects of calcium channel blockers, by increasing smooth muscle contraction and systemic vascular resistance, and subsequently blood pressure. In our case, this was supported by the observed reduction in vasopressor requirement to maintain mean arterial blood pressure.
Methylene blue has a relatively low risk safety profile and is considered safe in doses less than 2 mg/kg [11]. The dose and safety of a repeated dose are unclear but a single dose of 1.5–2 mg/kg of methylene blue seem to be safe [11]. Side effects appear to be transient and include skin and urine discoloration and interference with pulse oximetry reading giving a falsely depressed reading [11]. Anaphylactic reaction to methylene blue is possible but rare. Due to the risk of hemolysis, methylene blue is contraindicated in patients with glucose-6-phoshate deficiencies or severe renal failure [11]. Our patient had no absolute contraindications to administration and the only observed side effect was blue discoloration of the urine which lasted less than 24 hours after administration of methylene blue.
A potential concern with the use of methylene blue is that it is a partial inhibitor of monoamine oxidase, and thus the simultaneous use with serotonergic agents is cautioned due to the risk of development of serotonin syndrome [12]. Our patient took a polypharmacy overdose which included citalopram, a selective serotonin reuptake inhibitor. The risk of serotonin syndrome was appreciated but given the low dose of substance ingested, the risk was deemed low. Given the patient had been mechanically ventilated and all functions were monitored the appearance of a serotonergic syndrome would have been easily detected and treated accordingly.
Limitations to the interpretation of this case study includes the concomitant ingestion of multiple substances including CCB, selective serotonin reuptake inhibitor, 3-hydroxy-3-methylglutaryl coenzyme A (HMG CoA) reductase inhibitor and antihistamine. Distributive shock was assumed to be secondary to CCB as this was ingested in the most significant quantity and known to cause profound hypotension in large doses. However unlikely due to the small quantity ingested, the improvement in hemodynamic status could be secondary to citalopram which can cause hypertension in the setting of serotonin syndrome [13]. An argument can also be made that the patient was intubated for five days and therefore the improvement of the hemodynamic state could be due to the complete metabolism of the drug. This is difficult to demonstrate due to the slow release component of the drug ingested. Another limitation that we appreciate is that it may be difficult to distinguish whether hemodynamic stability would have been achieved with or without methylene blue administration.
To our knowledge, currently, there are no randomized control trials to support its use in CCB overdose, and evidence is currently limited to observational studies in the form of single case reports. In 2019, Ahmed and Barnes reported similar benefits of methylene blue administration in the case of amlodipine overdose [14]. Pasin et al. conducted a meta-analysis of randomized trials evaluating the efficacy of methylene blue on raising mean arterial pressure in distributive shock in ICU patients with sepsis, patients’ post-cardiac and liver transplant surgery [15]. The observed effect was an increase in mean arterial pressure in patients receiving methylene blue with a mean of 6.93 mmHg (95% CI 1.67–12.18, p = 0.01) [15]. Porizka et al. conducted a retrospective study evaluating the hemodynamic effectiveness of methylene blue used in refractory shock in critically ill patients [16]. Following a single bolus of methylene blue, 45% of patients responded with a reduction of vasopressor requirement within 2 hours and had reduced mortality rates [16]. The researchers also proposed that methylene blue is given early in shock, before refractory shock, and profound tissue ischemia is established [16].
Given that the current expert consensus on the treatment of refractory shock secondary to CCB overdose is based on relatively low-level evidence, we suggest that the use of methylene blue also be considered, not as a rescue therapy but as an adjunct to first-line therapy [5]. Not only can it produce a hemodynamic benefit in such cases, but it is also relatively cheap and readily available and has a low risk safety profile [7]. This case report supports the hypothesis that methylene blue can assist in achieving hemodynamic stability in CCB overdose.
CONCLUSION
Calcium channel blocker overdose can be fatal as it is associated with severe distributive shock. Conventional treatment for symptomatic overdose includes IV calcium, high dose insulin therapy, and vasopressors. Some patients may fail first-line therapies, described as “refractory shock.” We propose the use of methylene blue in CCB overdose as an adjunct therapy to current first line therapy before refractory shock is established.
REFERENCE
1.
Cioccari L, Luethi N, Bailey M, Pilcher D, Bellomo R. Characteristics and outcomes of critically ill patients with drug overdose in Australia and New Zealand. Crit Care Resusc 2017;19(1):14–22.
[Pubmed]

2.
Savage M, Kung R, Green C, Thia B, Perera D, Tiruvoipati R. Predictors of ICU admission and long-term outcomes in overdose presentations to Emergency Department. Australas Psychiatry 2020;28(1):75–7. [CrossRef]
[Pubmed]

3.
Ramoska EA, Spiller HA, Winter M, Borys D. A one-year evaluation of calcium channel blocker overdoses: Toxicity and treatment. Ann Emerg Med 1993;22(2):196–200. [CrossRef]
[Pubmed]

4.
Levine M, Curry SC, Padilla-Jones A, Ruha AM. Critical care management of verapamil and diltiazem overdose with a focus on vasopressors: A 25-year experience at a single center. Ann Emerg Med 2013;62(3):252–8. [CrossRef]
[Pubmed]

5.
St-Onge M, Anseeuw K, Cantrell FL, et al. Experts consensus recommendations for the management of calcium channel blocker poisoning in adults. Crit Care Med 2017;45(3):e306–15. [CrossRef]
[Pubmed]

6.
Kwok ESH, Howes D. Use of methylene blue in sepsis: A systematic review. J Intensive Care Med 2006;21(6):359–63. [CrossRef]
[Pubmed]

7.
Jang DH, Nelson LS, Hoffman RS. Methylene blue for distributive shock: A potential new use of an old antidote. J Med Toxicol 2013;9(3):242–9. [CrossRef]
[Pubmed]

8.
Ignarro LJ, Kadowitz PJ. The pharmacological and physiological role of cyclic GMP in vascular smooth muscle relaxation. Annu Rev Pharmacol Toxicol 1985;25:171–91. [CrossRef]
[Pubmed]

9.
Leyh RG, Kofidis T, Strüber M, et al. Methylene blue: The drug of choice for catecholamine-refractory vasoplegia after cardiopulmonary bypass? J Thorac Cardiovasc Surg 2003;125(6):1426–31. [CrossRef]
[Pubmed]

10.
11.
Ginimuge PR, Jyothi SD. Methylene blue: Revisited. J Anaesthesiol Clin Pharmacol 2010;26(4):517–20.
[Pubmed]

12.
Ng BKW, Cameron AJD. The role of methylene blue in serotonin syndrome: A systematic review. Psychosomatics 2010;51(3):194–200. [CrossRef]
[Pubmed]

13.
Boyer EW, Shannon M. The serotonin syndrome. N Engl J Med 2005;352(11):1112–20. [CrossRef]
[Pubmed]

14.
Ahmed S, Barnes S. Hemodynamic improvement using methylene blue after calcium channel blocker overdose. World J Emerg Med 2019;10(1):55–8. [CrossRef]
[Pubmed]

15.
Pasin L, Umbrello M, Greco T, et al. Methylene blue as a vasopressor: A meta-analysis of randomised trials. Crit Care Resusc 2013;15(1):42–8.
[Pubmed]

16.
Porizka M, Kopecky P, Dvorakova H, et al. Methylene blue administration in patients with refractory distributive shock – a retrospective study. Sci Rep 2020;10(1):1828. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Annica Bester - Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Margareta A Roeck - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Annica Bester et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.