|
Case Report
Atlantoaxoid subluxation by suboccipital Pott's disease: Arthrodesis using the Harms technique. About a case and review of the literature
1 Neurosurgery Department, Fann University Hospital, Dakar, Senegal
Address correspondence to:
Louncény Fatoumata Barry
MD, Neurosurgery Department, Fann University Hospital, Post Box: 5035, Dakar,
Senegal
Message to Corresponding Author
Article ID: 100088Z06MF2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Faye M, Barry LF, Diop A, Sy ECN, Cisse Y, Badiane SB. Atlantoaxoid subluxation by suboccipital Pott’s disease: Arthrodesis using the Harms technique. About a case and review of the literature. Case Rep Int 2020;9:100088Z06MF2020.ABSTRACT
Introduction: The suboccipital location of Pott′s disease is exceptional, and may be complicated by compression of the bulbomedullary junction.
Case Report: We report the case of a young patient of 32 years of age, received in a table of spastic tetraplegia preceded by cervicalgia without associated sensory or sphincter disorders. Computed tomography and magnetic resonance imaging of the cervico-occipital hinge showed C1-C2 subluxation with osteolysis of the C1 arches, bone sequestration, and anterior compression of the bulbomedullary junction, requiring arthrodesis using the Harms technique. Diagnostic confirmation was obtained by pathological examination of bone fragments and epidural tissue removed per operation. Tuberculosis chemotherapy was started for 16 months. Progression was favorable with motor recovery allowing unaided walking.
Conclusion: The surgical indication of these all tuberculosis localizations depends on the presence of bulbomedullary compression and/or cervico-occipital hinge instability.
Keywords: Arthrodesis, Harms, Pott′s disease, Suboccipital
INTRODUCTION
Suboccipital Pott’s disease is extremely rare [1],[2]. It is an exceptional localization with an estimated frequency of less than 1% of all spinal tuberculosis localizations [1],[3],[4]. This localization of spinal tuberculosis can lead to instability and serious bulbomedullary complications [4].
The therapeutic indications depend on the extent of the lesions, the presence of a C1-C2 subluxation and the existence of associated neurological disorders [3]. Described in 2001, the Harms technique is the most recent of the C1-C2 arthrodesis techniques [5].
It is based on the fixation of C1 lateral masses and C2 pedicles using polyaxial screws, allowing a reduction in C1-C2 dislocations.
We report a case of suboccipital Pott’s disease, complicated by C1-C2 instability and treated surgically with the Harms technique and an antituberculosis drug.
CASE REPORT
This is a case of a 32-year-old patient with a history of pulmonary tuberculosis treated and declared cured in 2013, who presented five years later (2018) with neck pain followed by progressive tetraplegia of progressive onset over eight months.
The clinical examination found a patient with no change in general condition with spastic tetraplegia at brachial predominance (1/5 upper limbs and 2/5 lower limbs) without sensory disturbances or associated sphincterials classified as Frankel B. There was no cervical lymphadenopathy or fever neither night sweats. The tuberculin intradermal reaction (TID) was positive and the C-reactive protein (CRP) was 120 mg/L.
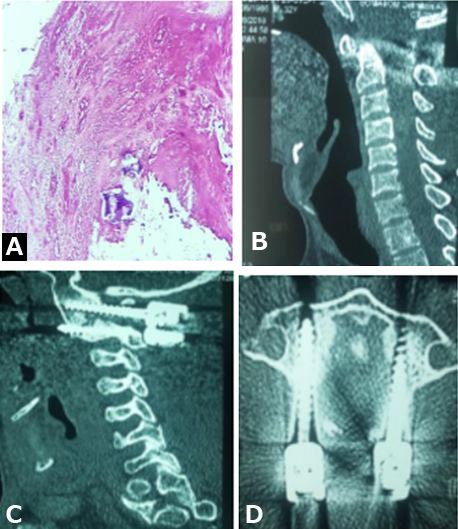
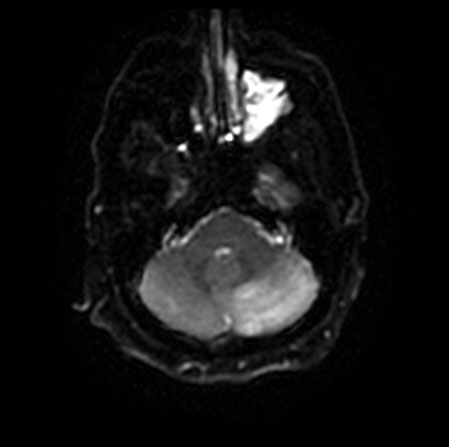
Computed tomography (CT) scan of the occipito-cervical hinge showed osteolysis of the odontoid, of the posterior arch and posterior wall of the anterior arch of C1 with C1-C2 subluxation and sequestration intracanal bone (see Figure 1). Magnetic resonance imaging (MRI) showed a compression of the bulbomedullary junction (Figure 1). C1-C2 requiring posterior arthrodesis by the Harms technique with laminectomy of C1 and removal of inflammatory bone tissue, and epidurals whose pathological examination revealed a gigantocellular epitheloid granuloma: Langhans cells (Figure 2), confirming the diagnosis of tuberculosis. Treatment with quadruple tuberculosis chemotherapy was initiated for four months followed by dual therapy for twelve months. The postoperative cervical CT scan showed a reduction in C1-C2 dislocation (see Figure 2).
Progression after tuberculosis treatment was marked by motor recovery allowing the walk (Frankel D).
DISCUSSION
Despite the high frequency of osteoarticular and especially spinal tuberculosis in developing countries, suboccipital Pott’s disease remains exceptional [6]. It is a rare and unusual condition. It is a serious localization due to the instability of the cervico-occipital hinge that it can cause and the resulting vital and neurological risk [7]. Usually it affects young adult males, as in the case of our patient [1],[7]. The clinical presentation is unspecific. It may be a clinic manifestation of common cervical pain, generally posterior, most often asymmetrical, with irradiation toward the occipital region, the ear and the upper limb [4]. This lateralization would correspond to a predominant involvement of a lateral mass. Cervical stiffness is classically found in nearly 80% cases [2] and is absent in our patient. Sometimes it is a more serious clinic manifestation of spinal cord compression at the origin of tetraparesis or tetraplegia, which can be rapidly progressive or insidious depending on the mechanism involved [4],[6]. The pathophysiology of these neurological disorders is explained by three factors: dislocation of C1-C2 by rupture or uninsertion of the transverse ligament, the basilar impression due to the separation of the lysed lateral masses, the extension of a cold abscess in the epidural [8]. In the case of our patient, tetraplegia was secondary to a C1-C2 dislocation with compression of the bulbomedullary junction by the odontoid. For some authors, it is rather the inflammatory process that is at the origin of these disorders, which explains the regression of neurological signs without decompression in some patients [2],[7] [8]. Atlantoaxoid tuberculosis can also be expressed by psychiatric disorders [9], or by ear, nose, and throat (ENT) disease: XII paralysis can occur in 3.5% cases and dysphagia in 12.5% cases [4], it is due to a retropharyngeal abscess which can also cause dysphonia and dyspnea.
In terms of imaging, the radiological data are used to guide the diagnosis. At the beginning of the evolution, semiology is discrete, because of the difficulties of interpretation of conventional radiology, origin of a great diagnostic delay exposing them to the risk of spinal cord compression. In profile, two signs should alert: the loss of parallelism of the lower edge of the posterior arch of C1 and of the upper edge of the spinous process of C2, and in front of the increase of the retropharyngeal fatty space. The retropharyngeal fat space should not exceed 7–10 mm. Otherwise, a prevertebral abscess will occur [4],[6]. In our case, the imaging mainly involved CT and MRI. They allow a better analysis of the extent of the lesions. It is also used for therapeutic follow-up [2]. Spiral CT, in axial sections with contrast injection, allows precise definition of the lesions whether they are bony, discal, or adjacent soft tissues. On the bone windows, atlantoaxoid osteolytic lesions with posterolateral dislocation of the odontoid present in 68% of cases [2], as in our patient’s case. Computed tomography remains of great interest in the search for bone sequestration, within osteolysis and within epidural and paravertebral abscesses, which are highly suggestive of tuberculosis. The parenchymal windows show sheathing epiduritis and calcifications within the abscess foci. The latter can be large and may repress the aerodigestive tract [4],[9].
Magnetic resonance imaging has a sensitivity of 96% and specificity of 92% for infectious spondylodiscitis. It allows better visualization of soft tissue involvement, especially prevertebral collections and their intra- and extra-canal extension. The search for abscesses is of major diagnostic and prognostic interest [7]. These abscesses circumferentially fill the prevertebral, latero-vertebral, and posterior paraspinal regions. They appear on T1 and T2 weighted sagittal slices as a heterogeneous signal process (iso-hyposignal in T1 and hypersignal in T2), which is intensely enhanced after injection of contrast material. On the other hand, the bone signal of the lateral masses is hypo-intense in T1, hyper-intense in T2, and heterogeneously enhanced after injection of gadolinium, which makes it possible to better delimit osteolytic. Magnetic resonance imaging also shows atlantoaxoid dislocation and basilar impression due to ligament instability and epidural infiltration [2],[8].
Differential diagnoses are thus those of the destructive osteoarthritis associated with a mass of the adjacent soft parts. These are essentially infections with pyogens, rheumatoid arthritis, and joint chondrocalcinosis (CCA). These three pathologies have the particularity to be osteoarthritis rather than median, atlanto-odontoid, although the damage to the lateral joints is described [2].
Confirmation of the diagnosis is made by finding Koch bacilli in the abscess, or by CT or surgical biopsy. However, in endemic areas and where there are signs of presumption, bacteriological or histological confirmation no longer appears to be essential to institute antibacillary treatment. The diagnosis can be based on a number of converging arguments: the notion of tuberculosis contagion, the positivity of the intradermal reaction, the radiological aspect, the existence of other locations and the demonstration of Koch bacilli at a distance [8]. In our case, diagnostic confirmation was obtained by anatomopathological examination of bone samples from the posterior arch and epidural tissue obtained intraoperatively.
The treatment of suboccipital Pott’s disease is based on long-term multidrug therapy for tuberculosis, combined with immobilization of the cranio-spinal hinge to allow sedation of the pain and faster healing [8].
Medical treatment may be sufficient. All authors agree that emergency thoracocervical immobilization for five months to a year is necessary [4],[6],[9]. However, the extent of some bone destruction, its progressive nature, and the length of the reconstruction phase make the neck brace too uncomfortable and sometimes insufficient. Under these conditions, or if signs of progressive compression appear, surgical arthrodesis is indicated [4],[9]. The approach may be anterior, posterior, or combined. In our case, the arthrodesis was performed posteriorly using the Harms technique [5]. This atlantoaxoid arthrodesis technique uses screw fixation of the lateral masses of C1 and the pedicular masses of C2. It allows reduction of anteroposterior displacement between C1 and C2, but is complicated by the relationship with the Arnold’s nerve, venous plexus, and vertebral artery [10]. Retropharyngeal and epidural abscesses can be drained, if they are large, to speed healing [4]. The evolution is toward bone reconstruction with fusion and vertebral blocks. Standard X-rays show images of somatic condensations, vertebra plana, and vertebral block in parallel with healing. With MRI, the spinal signal normalizes within a few months in properly treated patients [2],[4].
CONCLUSION
The suboccipital location of tuberculosis is rare, and may be complicated by atloid-axoid dislocation with compression of the bulbomedullary junction responsible for tetraplegia. Computed tomography and MRI allow a good evaluation of osteoarticular and soft tissue lesions. The medical treatment associated with orthopedic treatment is generally sufficient to ensure consolidation. However, surgery is indispensable in forms with instability of the cervico-occipital hinge. The evolution is favorable in case of early diagnosis and adequate management.
REFERENCE
1.
Ousehal A, Gharbi A, Zamiati W, Saidi A, Kadiri R. Imaging findings in 122 cases of Pott’s disease. [Article in French]. Neurochirurgie 2002;48(5):409–18.
[Pubmed]

2.
Augier A, Zrig H, Roqueplan F, Brauner M, Dumas JL. MR and CT features of craniocervical junction tuberculosis: A report of 5 cases. [Article in French]. J Radiol 2008;89(5 Pt 1):585–9. [CrossRef]
[Pubmed]

3.
Gupta SK, Mohindra S, Sharma BS, et al. Tuberculosis of the craniovertebral junction: Is surgery necessary? Neurosurgery 2006;58(6):1144–50. [CrossRef]
[Pubmed]

4.
5.
Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976) 2001;26(22):2467–71. [CrossRef]
[Pubmed]

6.
7.
Ibahioin K, Ait Ben Ali A, Choukri M, et al. Suboccipital tuberculosis: A case report. [Article in French]. Neurochirurgie 2001;47(1):66–8.
[Pubmed]

8.
9.
Kanaan IU, Ellis M, Safi T, Al Kawi MZ, Coates R. Craniocervical junction tuberculosis: A rare but dangerous disease. Surg Neurol 1999;51(1):21–6. [CrossRef]
[Pubmed]

10.
Bourdillon P, Perrin G, Lucas F, Debarge R, Barrey C. C1-C2 stabilization by harms arthrodesis: Indications, technique, complications and outcomes in a prospective 26-case series. Orthop Traumatol Surg Res 2014;100(2):225–31. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Mohameth Faye - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Louncény Fatoumata Barry - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Abdoulaye Diop - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Elhadj Cheikh Ndiaye Sy - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Yakhya Cisse - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Seydou Boubakar Badiane - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Mohameth Faye et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.