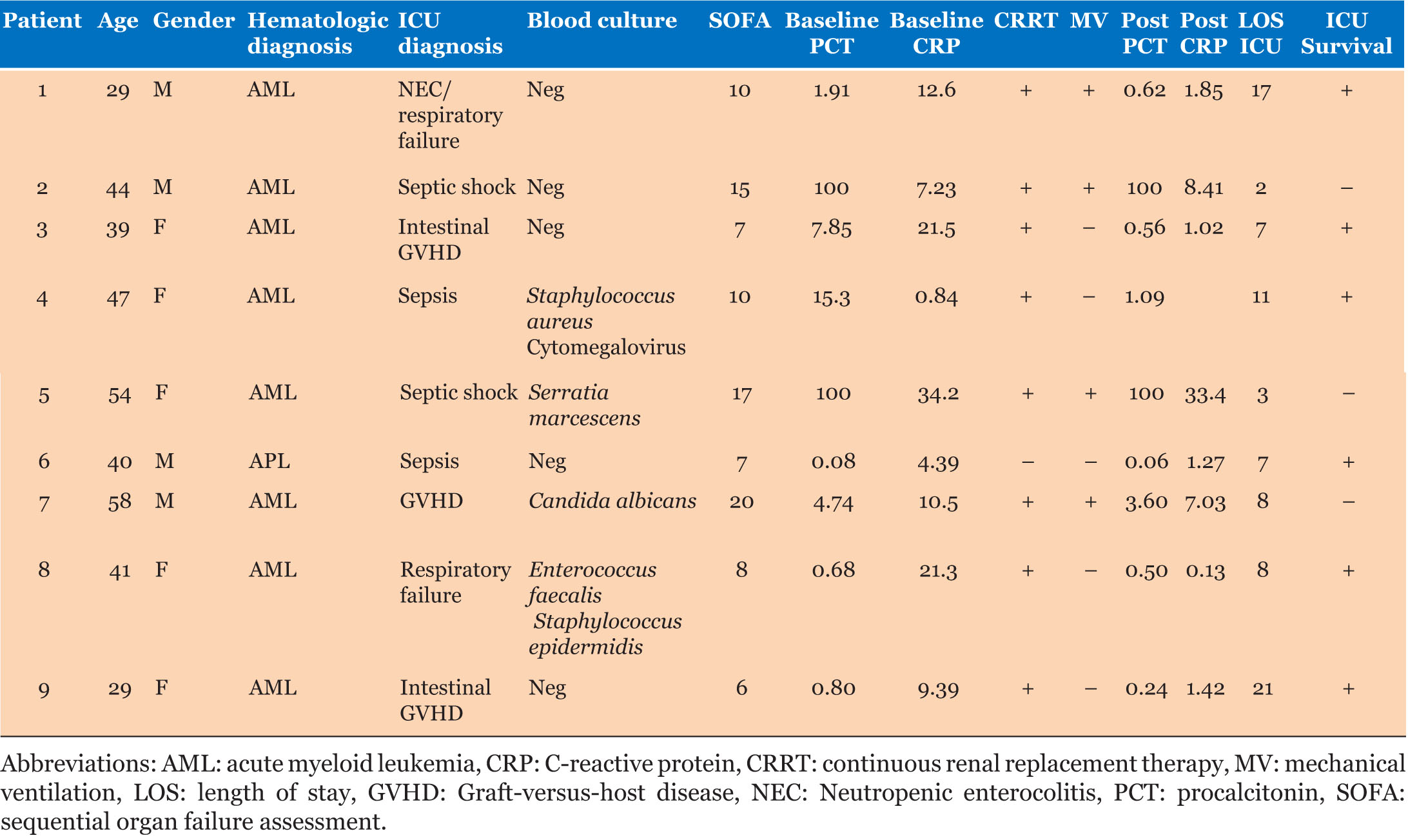
|
Case Report
Cutaneous metastatic lesion as a presentation of rectal cancer: A case report
1 Hospital Dr. Nélio Mendonça – Resident, General Surgery Department, Funchal, Madeira, Portugal
2 Hospital Dr. Nélio Mendonça – Consultant, General Surgery Department, Funchal, Madeira, Portugal
Address correspondence to:
Catarina Muller
Avenida Luís de Camões, Nº 47, Funchal, Madeira, Postal Code: 9004-514,
Portugal
Message to Corresponding Author
Article ID: 100097Z06CM2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Muller C, Rodrigues C, Gouveia M, Encarnação V, Sousa MO, Reis M. Cutaneous metastatic lesion as a presentation of rectal cancer: A case report. Case Rep Int 2021;10:100097Z06CM2021.ABSTRACT
Introduction: Colorectal cancer is ranked third among the most commonly diagnosed malignancies and second among the leading causes of cancer death in the world. However, only a few case reports are found in the literature regarding skin metastases originating from rectal cancer, which usually shows widespread disease and poor prognosis.
Case Report: A 68-year-old female patient presented with anterior chest wall pain and swelling and a history of progressive growing of the lesion for the last five months. Physical examination revealed a palpable 3 cm mass in the intermammillary area with mild inflammation of the surrounding skin. The lesion biopsy revealed moderately differentiated intestinal-type adenocarcinoma, suggesting metastasis of a colorectal primary cancer. Colonoscopy revealed an obstructive neoplasm of the rectum located 12 cm from the anal verge. Histology revealed a moderately differentiated adenocarcinoma as seen before in the skin lesion. The computed tomography (CT) scan also detected several secondary lesions on the liver.
Conclusion: Approximately 0.8% of the patients present with a skin lesion as the first indication of a silent internal malignancy, which is rare and carries a poor prognosis. Cutaneous metastases are considered as an advanced presentation of colorectal cancer, mostly managed with palliative care.
Keywords: Colorectal cancer, Cutaneous metastases, Skin lesion
INTRODUCTION
Colorectal cancer (CRC) is a globally important public health issue. According to data published by World Health Organization, the CRC is ranked third among the most commonly diagnosed malignancies and second among the leading causes of cancer death in the world. More than 10% of cases are already metastatic tumors by the time they are diagnosed. The sites most often affected by the advanced disease are the liver, lungs, and central nervous system [1]. It is extremely rare to encounter cutaneous metastases from colorectal cancer. Presence of cutaneous metastases indicates poor prognosis and widespread of disease [2],[3].
The authors present a clinical case of a skin lesion as a presentation of rectal cancer.
CASE REPORT
The authors present a case of a 68-year-old female with a personal history of appendectomy for acute appendicitis, with no relevant comorbidities, medication, or family background of oncological diseases.
The patient was admitted to the emergency department with anterior chest wall pain and swelling and a history of progressive growing of the lesion for the last five months. Physical examination revealed a palpable 3 cm mass in the intermammillary area with mild inflammation of the surrounding skin. The patient was discharged with a prescription of oral antibiotics and a diagnosis of an infected sebaceous cyst. A week later she was reassessed and significant growth of the mass was detected (5 cm) at the physical exam with inflammatory signs, starting suspicious ulceration as well as hemato-purulent discharge (Figure 1). The patient was then admitted to the General Surgery department for intravenous therapy and additional diagnostic exams.
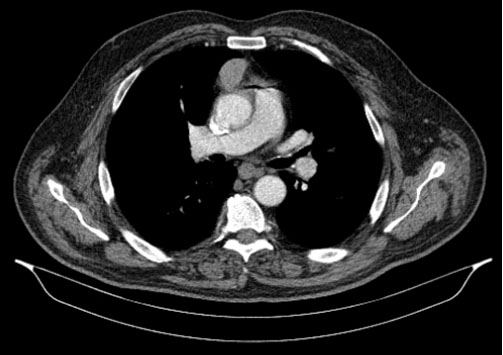
Within a week the lesion grew ulcerated (Figure 2). Skin biopsy revealed moderately differentiated intestinal-type adenocarcinoma and immunohistochemistry markers revealed positive for CK20 and negative for CK7, suggesting metastases of a colorectal primary cancer. During her hospital stay, she developed rectal bleeding episodes associated with constipation that reaffirmed a need for an endoscopy study. Colonoscopy showed an obstructive neoplasm of the rectum located 12 cm from the anal verge (Figure 3). Histology revealed a moderately differentiated adenocarcinoma as seen before in the skin lesion, with the presence of the P.GLY13ASP (C.38G>A) mutation in the KRAS gene. The cancer staging was completed with a thoracic, abdominal, and pelvic CT scan, which described the rectal mass as a concentric thickening of the rectum with 12 cm of extension involving the sigmoid transition. The intermammary metastasis was referred as a solid nodular lesion of the pre-sternal soft tissue, with approximately 49 × 48 mm and with contrast enhancement (Figure 4). The CT scan also detected several secondary lesions on the liver, with special emphasis on the ones in the transition of the II/III segment (45 mm), segment VI (67 mm), and segment VII (22 mm).
A derivative colostomy was proposed in multidisciplinary team discussion, along with palliative hemostatic radiotherapy to the rectum and skin metastasis in addition to systemic chemotherapy. The palliative treatment improved rectorragia, with stable hemoglobin values (11 g/dL) and no further need of blood transfusions. The cutaneous tumor remained dimensionally stable. Pain was controlled with medication.
DISCUSSION
Cutaneous metastases of cancer are rare, occurring in about 1.3% of cases at the time of presentation of the primary tumor [2].The reported case shows a rather uncommon presentation with cutaneous metastasis being the very first manifestation of inaugural internal cancer. The high incidence of CRC makes it an accountable source of metastases to the skin. Nonetheless, patients with this clinical finding represent only 4% of all patients diagnosed with CRC, making it a rare diagnostic [4].
In these cases, cutaneous metastases can assume a plethora of morphologic characteristics. Although nodules and cutaneous tumors are the most recurrent forms, inflammatory tissue responses such as cellulitis can be present—both patterns were observed in our patient [4],[5]. Several other forms of presentation are described in literature such as ulcers, blisters, alopecia plaques, and lesions that resemble herpes-zoster, epidermal cysts, neurofibromas, lymphomas, annular erythema, condylomas, and elephantiasis nostras verrucosa, among others [4],[5],[6].
The most common presentation of rectal carcinoma’s skin metastases is as small subcutaneous or intradermal nodules measuring 1–2 cm in diameter. Even though there aren’t any distinctive feature regarding these, they tend to coalesce. These lesions are usual asymptomatic, firm, rubbery, and painless [7],[8].
Distance to the primary tumor plays a major role in influencing sites in which cutaneous metastases appear. The closer the skin is to the primary tumor, higher is the chance of metastases. Thus, making the abdominal wall the most affected site in the case of CRC. Either direct extension of the primary tumor, hematogenic or lymphatic dissemination can influence this process [3],[4],[5]. This also explains why locations such as the pelvis, torso, thorax, upper extremities, head, neck, and upper lip are rarely affected sites by cutaneous metastases [9],[10].
Histopathology helps in establishing the correct diagnosis. Microscopical findings show similar features in both the primary tumor and the metastatic lesions. The most common type of large bowel tumors with cutaneous metastases is well differentiated mucin-secreting adenocarcinomas [3].The immunohistochemical study is of the outmost importance in histopathological studies. The pattern of CK7-negative/CK20-positive pattern is presented in more than 70% cutaneous metastases from CRC [5].
Pathology findings in the present report showed a cutaneous metastases of an intestinal pattern moderately differentiated adenocarcinoma–immunohistochemical profile: CK7− and CK20+.
The treatment of cutaneous metastases is immediately palliative, with surgical resection reserved for solitary lesions [1],[5]. Radiotherapy and chemotherapy can be used for the palliation of local symptoms.
Once diagnosed, the cutaneous metastasis typically represents widespread disease and a reserved prognosis: more than two-thirds of patients will die within the first six months [5]. Nevertheless, there are quite a few described cases which present themselves with isolated rectal metastases to the skin without any other signs of spread disease [11],[12].
CONCLUSION
It is uncommon to find cutaneous metastases as a presentation of a rectal carcinoma. These lesions are often accompanied by visceral metastases at presentation, reflecting advanced disease, and mostly managed with palliative care.
REFERENCE
1.
Wong NS, Chang BM, Toh HC, Koo WH. Inflammatory metastatic carcinoma of the colon: A case report and review of the literature. Tumori 2004;90(2):253–5.
[Pubmed]

2.
Wang DY, Ye F, Lin JJ, Xu X. Cutaneous metastasis: A rare phenomenon of colorectal cancer. Ann Surg Treat Res 2017;93(5):277–80. [CrossRef]
[Pubmed]

3.
Nesseris I, Tsamakis C, Gregoriou S, et al. Cutaneous metastasis of colon adenocarcinoma: Case report and review of the literature. An Bras Dermatol 2013;88:56–8. [CrossRef]
[Pubmed]

4.
Lookingbill DP, Spangler N, Helm KF. Cutaneous metastases in patients with metastatic carcinoma: A retrospective study of 4020 patients. J Am Acad Dermatol 1993;29(2 Pt 1):228–36. [CrossRef]
[Pubmed]

5.
Saeed S, Keehn CA, Morgan MB. Cutaneous metastasis: A clinical, pathological, and immunohistochemical appraisal. J Cutan Pathol 2004;31(6):419–30. [CrossRef]
[Pubmed]

6.
7.
Reingold IM. Cutaneous metastases from internal carcinoma. Cancer 1966;19(2):162–8. [CrossRef]
[Pubmed]

8.
Rendi MH, Dhar AD. Cutaneous metastasis of rectal adenocarcinoma. Dermatol Nurs 2003;15(2):131–2.
[Pubmed]

9.
Góes HF, Lima Cdos S, Souza MB, Estrella RR, Faria MA, Rochael MC. Single cutaneous metastasis of colon adenocarcinoma – Case report. An Bras Dermatol 2016;91(4):517–9. [CrossRef]
[Pubmed]

10.
Moonda A, Fatteh S. Metastatic colorectal carcinoma: An unusual presentation. J Cutan Pathol 2009;36(1):64–6. [CrossRef]
[Pubmed]

11.
Ozgen A, Karakaya E, Bozdoğan N. Scrotal skin metastasis from rectum adenocarcinoma. Rare Tumors 2013;5(4):e60. [CrossRef]
[Pubmed]

12.
Reuter J, Bruckner-Tuderman L, Braun-Falco M. Epidermotropic scrotal metastasis of colorectal cancer. Int J Colorectal Dis 2007;22(9):1133–4. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgement
António Caires, Hospital Dr. Nélio Mendonça – Resident, General Surgery Department, Funchal, Madeira, Portugal, cairesgirao@hotmail.com
Diana Fernandes, Hospital Dr. Nélio Mendonça – Consultant, General Surgery Department, Funchal, Madeira, Portugal, dianarfernandes@gmail.com
Rómulo Ribeiro, Hospital Dr. Nélio Mendonça – Consultant, General Surgery Department, Funchal, Madeira, Portugal, romuloribeiro@live.com.pt
Jorge Fernandes, Hospital Dr. Nélio Mendonça – Consultant, General Surgery Department, Funchal, Madeira, Portugal, jorgemfernandes@hotmail.com
Ricardo Viveiros, Hospital Dr. Nélio Mendonça – Consultant, General Surgery Department, Funchal, Madeira, Portugal, ricardoviveiros@hotmail.com
Fernando Jasmins, Hospital Dr. Nélio Mendonça – Consultant, General Surgery Department, Funchal, Madeira, Portugal, ftgj55@gmail.com
Catarina Muller - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Catarina Rodrigues - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Manuel Gouveia - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Vítor Encarnação - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Maria Olim Sousa - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Miguel Reis - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Catarina Muller et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.