|
Case Report
Happy hypoxic: Unaware young man with DVTs and pulmonary emboli
1 Resident Physician, Internal Medicine, Northeast Georgia Medical Center, Gainesville, GA, USA
2 Assistant Clinical Professor of Medicine, AU/UGA Medical Partnership, Gainesville, GA, USA
Address correspondence to:
Christine Sykalo
DO, 743 Spring St. NE, Suite 710, Gainesville, GA 30501,
USA
Message to Corresponding Author
Article ID: 100102Z06CS2021
Access full text article on other devices
Access PDF of article on other devices

How to cite this article
Sykalo C, Arfoosh R. Happy hypoxic: Unaware young man with DVTs and pulmonary emboli. Case Rep Int 2021;10:100102Z06CS2021.ABSTRACT
Introduction: COVID-19 is a multi-systemic disease announced to be a pandemic by the WHO within three months of the first reported case. It was initially characterized as a respiratory virus; however, hypercoagulability and development of strokes and deep vein thrombosis (DVTs) have been seen. We present a case of a young patient with no past medical history who developed minimally symptomatic bilateral DVTs and pulmonary emboli (PE).
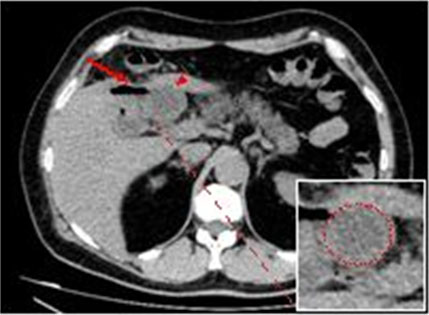
Case Report: A 26-year-old male with no past medical history presented with complaints of cough, fever, and diarrhea. Symptoms started two weeks prior to presentation, and he tested negative on COVID-19 nasal swab within that time frame. His cough was improving; however, he developed inability to keep food down along with bilateral calf pain with ambulation for three days prior to admission. Admission vitals were notable for fever and oxygen saturation of 91% on room air. A duplex ultrasound of the lower extremities showed bilateral thrombosis. Pulmonary computed tomography angiography (CTA) showed bilateral pulmonary emboli with numerous filling defects in the pulmonary arteries, along with peripheral interstitial densities. His COVID-19 nasal swab polymerase chain reaction (PCR) was negative, but the IgG serum antibody was positive. He was treated with steroids and anticoagulation.
Conclusion: Studies have documented that patients with COVID-19 pneumonia have increased risk of lower limb DVT, despite proper prophylactic treatment. Clinicians must maintain high index of suspicion and a low threshold to order key tests in setting of unexplained hypoxia. We recommend obtaining serologic studies in late presenting patients with negative PCR swabs.
Keywords: COVID-19, Pulmonary emboli, SARS-CoV-2, Venous thrombosis, Young adult
INTRODUCTION
The coronavirus disease 2019, also known as COVID-19, is a multi-systemic disease [1], which was announced to be a pandemic by the World Health Organization within three months of the first reported case [2]. COVID-19 was initially characterized as a respiratory virus, causing pneumonia and acute respiratory failure. The first autopsies reported that patient laboratory analyses were notable for elevated d-dimer, ferritin, fibrinogen, prothrombin time (PT), and, within 24 hours of death, an increased neutrophil count with relative lymphopenia [3]. The virus was seen to affect multiple organ systems, and was also recognized for its vascular effects. Additionally, articles are now being published on the ongoing symptoms patients experience from COVID-19, and include effects on brain, eyes, skin, and joints [4].
Vascular effects of COVID-19 were recognized initially in critically ill patients; however, hypercoagulability and development of strokes and deep vein thrombosis (DVTs) have been seen in non-critically ill patients with COVID-19 as well [5],[6]. Here, we present a case of a young patient with no past medical history who developed minimally symptomatic bilateral DVTs and pulmonary emboli (PE).
CASE REPORT
A 26-year-old male with no known past medical history presented with complaints of cough, fever, and diarrhea. The patient reported working as a landscaper. Two weeks prior to admission, he was at a party, where he drank about one bottle of tequila. He went to work the next day, felt ill, and requested to go home. The patient developed a cough, which was followed by a fever, and then diarrhea. In terms of his close contacts, the patient’s mother had a recent upper respiratory illness as well, but she recovered with no medical intervention. The patient did get tested for COVID-19 by nasal swab during his illness, but the results came back negative. The patient reported that his diarrhea was only one loose stool per day. His cough was reported to be non-productive, and he denied any wheezing or hemoptysis. His cough was improving; however, he began developing vomiting after meals two days prior to his admission. He decided to come to the emergency department (ED) because of inability to keep food down. Additionally, he reported bilateral mid-calf pain with ambulation for three days prior to admission, and denied any shortness of breath. He had cough, diarrhea, and fevers for two weeks prior to developing of calf pains.
The patient denied any personal history of clotting or lung disorders, and denied any known diagnoses. He reported no family health issues, except for mother’s recent illness, which had cleared. No known family history of hypertension, lung disease, clotting disorders, or strokes was found. Additionally, he denied any tobacco abuse, and admitted to trying methamphetamine once, two years prior. His social history was only notable for binge drinking at parties several times a month.
The vital signs of the patient were all within normal limits, except for a fever of 38.1°C and oxygen saturation of 91% on room air. He was placed on 1–2 liters of oxygen via nasal cannula, which improved his saturation to 100%. On physical exam, the patient was pleasant and cooperative, without increased work of breathing. He was comfortable speaking in full sentences. On auscultation, heart sounds were regular rate and rhythm, without any murmurs. He did have fine inspiratory crackles at the bilateral bases, left more than right. Abdominal exam was unremarkable. Musculoskeletal exam was notable for dorsalis pedis pulses of +1/3, and cold feet. The patient had tenderness to palpation to midline of calves bilaterally, without signs of edema or erythema. Admission labs are shown in Table 1.
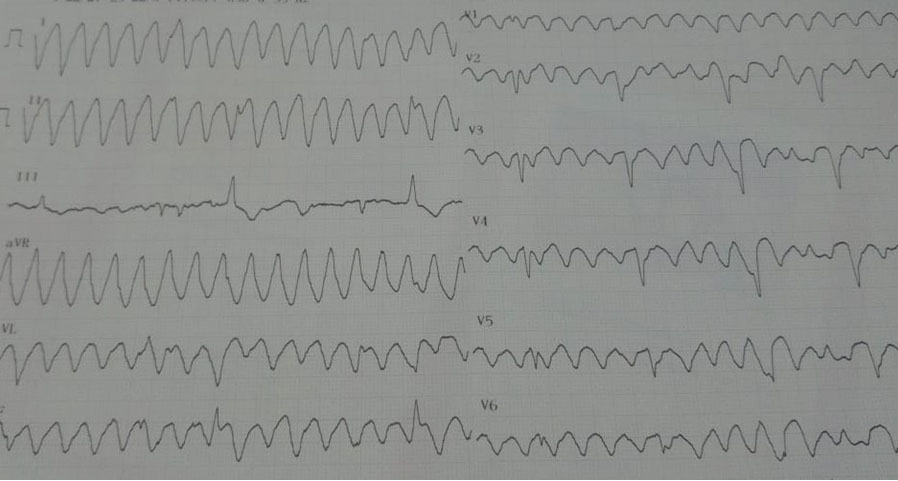
A duplex ultrasound of the bilateral lower extremities showed venous thrombosis of the bilateral posterior tibial veins and left peroneal vein. A transthoracic echocardiogram showed ejection factor of 55–60%, and normal size, wall thickness, and shape of ventricles and atria, without evidence of RV strain (Figure 1 and Figure 2).
The patient was started on a heparin drip, and he received intravenous dexamethasone for four days. He received only one day of Remdisivir, which was then stopped, as patient had significant improvement. He was weaned off supplemental oxygen, and discharged on apixaban and additional six days of 4 mg oral dexamethasone.
DISCUSSION
Studies have documented that non-critically ill patients with COVID-19 pneumonia have increased risk of lower limb DVT, despite proper prophylactic treatment. Of note, average age of the studied patients was 71.3, having multiple comorbidities, including hypertension, diabetes, and dyslipidemia [5]. Notably few reports have been published showing the effects of COVID-19 in patients under the age of 30, and the ones published, mostly show young patients to have strokes associated with COVID-19, frequently without an identifiable source for the stroke [6].
Other than age, timeline of illness is also of great importance, and detection rates vary. Serological testing has shown, during the second week of illness, that PCR is positive in 54.0% of patients, and antibody assays grow to be positive in 89.6% of patients, compared to 66.7% for PCR and 38.3% positive antibody assays during the first week of illness [7]. It is important to recognize that late presenting patients, such as ours, are much more likely to test negative by PCR, and require high index of suspicion and additional testing for proper diagnosis. This is also supported by current Infectious Diseases Society of America (IDSA) guidelines on the diagnosis of COVID-19 serologic testing as well as a systematic Cochrane Database review, showing that antibody testing, specifically IgG, is preferred after the two to three illness week period [8],[9].
Our patient developed coagulopathy after two weeks of illness with COVID-19, and recognition of late presentation was crucial for our patient. We were unable to identify other case reports of young patients, under the age of 30, with no co-morbidities, who were diagnosed with PE and DVT secondary to COVID-19. Our goal is to raise awareness of the vascular effects of COVID-19 specifically in the younger patient population. Specifically pointing out the development of calf pain from DVT’s after 11–14 days of illness, once the patient already had developed IgG antibodies.
Additionally, we would like to urge providers to do alcohol screening on all patients during the pandemic, as there has been a notable increase in alcohol consumption in US adults during this time [10]. There is no data available showing alcohol abuse to have worse prognosis of COVID-19 illness; however, this was the only known concern in the patient’s history.
CONCLUSION
In conclusion, COVID-19 is still currently active, and continues to be a threat to the lives and health of people across the globe. We would like to raise awareness of the effects it can have on seemingly healthy and young individuals, and recommend having a high index of suspicion of PE in patients with acute hypoxic respiratory failure, even if they lack other classic symptoms. Finally, we urge providers to hold open discussions with patients on topics of mental health and alcohol abuse, especially during the vulnerable times of the pandemic.
REFERENCE
1.
Temgoua MN, Endomba FT, Nkeck JR, Kenfack GU, Tochie JN, Essouma M. Coronavirus disease 2019 (COVID-19) as a multi-systemic disease and its impact in low- and middle-income countries (LMICs). SN Compr Clin Med 2020;1–11. [CrossRef]
[Pubmed]

2.
Listings of WHO’s response to COVID-19. World Health Organization. 2020. [Available at: https://www.who.int/news/item/29-06-2020-covidtimeline]

3.
Fox SE, Akmatbekov A, Harbert JL, Li G, Quincy Brown J, Vander Heide RS. Pulmonary and cardiac pathology in African American patients with COVID-19: An autopsy series from New Orleans. Lancet Respir Med 2020;8(7):681–6. [CrossRef]
[Pubmed]

4.
5.
Jimenez-Guiu X, Huici-Sánchez M, Rmera-Villegas A, Izquierdo-Miranda A, Sancho-Cerro A, Vila-Coll R. Deep vein thrombosis in noncritically ill patients with coronavirus disease 2019 pneumonia: Deep vein thrombosis in nonintensive care unit patients. J Vasc Surg Venous Lymphat Disord 2021;9(3):592–6. [CrossRef]
[Pubmed]

6.
Oxley TJ, Mocco J, Majidi S, et al. Large-vessel stroke as a presenting feature of COVID-19 in the young. N Engl J Med 2020;382(20):e60. [CrossRef]
[Pubmed]

7.
Zhao J, Yuan Q, Wang H, et al. Antibody responses to SARS-COV-2 in patients with novel coronavirus disease 2019. Clin Infect Dis 2020;71(16):2027–34. [CrossRef]
[Pubmed]

8.
Bhimraj A, Morgan RL, Shumaker AH, et al. Infectious diseases society of america guidelines on the treatment and management of patients with COVID-19. Clin Infect Dis 2020;ciaa478. [CrossRef]
[Pubmed]

9.
Deeks JJ, Dinnes J, Takwoingi Y, et al. Antibody tests for identification of current and past infection with SARS-COV-2. Cochrane Database Syst Rev 2020;6(6):CD013652. [CrossRef]
[Pubmed]

10.
Pollard MS, Tucker JS, Green HD Jr. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw Open 2020;3(9):e2022942. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Christine Sykalo - Conception of the work, Design of the work, Acquisition of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Rami Arfoosh - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementVerbal informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Christine Sykalo et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.