|
Case Report
Acute esophageal necrosis: A case report
1 Hospital Dr. Nélio Mendonça – Resident, General Surgery Department, Funchal, Madeira, Portugal
2 Hospital Dr. Nélio Mendonça – Consultant, General Surgery Department, Funchal, Madeira, Portugal
3 Centro Hospitalar Universitário de São João – Resident, General Surgery Department, Porto, Portugal
4 Centro Hospitalar Universitário de São João – Consultant, General Surgery Department, Porto, Portugal
Address correspondence to:
Catarina Muller
Avenida Luís de Camões, Nº 47, Funchal, Madeira, Postal Code: 9004-514,
Portugal
Message to Corresponding Author
Article ID: 100104Z06CM2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Muller C, Viveiros R, Rodrigues S, Ferrão A, Barbosa E, Barbosa J. Acute esophageal necrosis: A case report. Case Rep Int 2022;11:100104Z06CM2022.ABSTRACT
Introduction: Acute esophageal necrosis (AEN) is a rare clinical entity, with a multifactorial etiopathogenesis and characterized by the presence of a black esophagus seen during the upper gastrointestinal (UGI) endoscopy.
Case Report: A 76-year-old man with AEN was presented, whose UGI endoscopy revealed circumferential necrosis throughout the entirety of the esophageal mucosa with concomitant preservation of gastric mucosa.
Conclusion: We present this case after considering the rarity of the disease and its characteristic endoscopic features, emphasizing the importance of early diagnosis and the establishment of a targeted treatment to the underlying causes.
Keywords: Acute esophageal necrosis, Black esophagus, Endoscopy, Gastrointestinal hemorrhage
INTRODUCTION
Acute esophageal necrosis (AEN), also referred to as black esophagus or acute necrotizing esophagitis, was first described in 1990 by Goldenberg [1]. It is a rare condition and, due to the presence of a black circumferential esophagus with or without exudate, potentially fatal disease. It is classically characterized by an upper gastrointestinal (UGI) endoscopy, which extends, either partially or totally, to the esophagogastric junction (EGJ) [2].
Although the etiology of this type of lesion is not fully understood, it is believed to be multifactorial response embedded in a primary mechanism of ischemia. The following are well-known risk factors for the development of AEN: male, advanced age, diabetes mellitus (DM), neoplasia, malnutrition, renal failure (RI), cardiovascular compromise, trauma, and thromboembolic phenomena [3],[4],[5].
The most characteristic clinical presentation is the presence of an UGI bleed as well as hematemesis and eventually melena [6],[7]. The diagnosis of AEN is endoscopic and lesion biopsy, even though recommended, is not imperative to confirm the diagnosis [8].
The overall mortality rate is mostly related to the underlying medical status and is tallied to almost 32% [7].
CASE REPORT
The authors present a case of a 76-year-old man with a history of type II DM, stage 5 chronic kidney disease under management with hemodialysis, two episodes of stroke and a history of peptic ulcer.
He was admitted to the hospital in his area of residence, with a clinical status of lipothymia, dark vomiting, and melena. He denied having a history of consumption of non-steroidal anti-inflammatory drugs, alcoholic beverages, or caustic products. Initially, the possibility of upper gastrointestinal bleeding was put forth and the patient was then transferred to our hospital given the need of frequent hemodialysis.
When the patient was admitted to our hospital, December 3rd, he was conscious, cooperative in some tasks and disoriented, drowsy, hypotensive (blood pressure (BP): 88/61 mmHg), with bleached mucous membranes, very dehydrated and with a globus abdomen without pain in the physical examination. There was one episode of melena (positive for the peroxidase test). The arterial blood gas (ABG) in air was altered only in lactate levels, revealing a hyperlactacidemia of 3.6. Analytically with hemoglobin (Hb) 11.5 g/dL, leukocytosis 19,010/mm3, urea 190 mg/dL, creatinine 10.1 mg/dL, myoglobin 2098, and polymerase chain reaction (PCR) 37.8 mg/dL. Study of coagulation was without any changes.
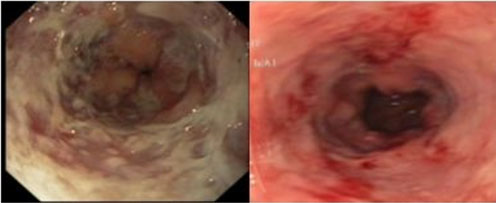
After attaining hemodynamic stability, with 1 U red blood cells and fluid therapy, a UGI endoscopy was preformed, which revealed circumferential necrosis of the whole esophageal mucosa with concomitant unaffected gastric mucosa (Figure 1). The contrasted computed tomography scan (CT scan) presented with circumferential thickening of the esophagus without parietal uptake, in reference to known necrosis (Figure 2).
The patient was admitted in the General Surgery Service and was medicated with fluid therapy, intravenous proton pump inhibitors (PPI) with continuous perfusion, broad spectrum antibiotics, nil-per-os, and scheduled hemodialysis.
During the course of the hospitalization, the patient did not present with new episodes of blood loss or required further transfusion. Due to malnutrition, he began parenteral nutrition, beginning an oral diet on the 11th day of hospitalization. He was subjected to analytical control and the hemodialysis sessions were scheduled in alternate days and were without complications. He repeated the UGI endoscopy on the 16th of December, revealing erythematous mucosa in the esophagus, with exudate, mucus, and friability, with no other changes (Figure 3). The patient was discharged after completing 17 days of hospitalization.
DISCUSSION
Acute esophageal necrosis is a rare clinical entity, first described in 1990 by Goldenberg et al. [1] with a prevalence of 0.01–0.2% among all UGI endoscopy and autopsies [9].
This condition shows a clear predilection in respect to gender and age. Men are four times more affected than women and, although the disease has been documented in all age groups, the peak incidence occurs in the sixth decade of life, averaging 67 years of age [7]. The presence of medical comorbidities including vascular disease, DM, hypertension, renal insufficiency, alcohol abuse, heart/lung disease, malnutrition, neoplasia, hypovolemic shock, strokes, infections (cytomegalovirus and herpes), sensitivity to antibiotics, gastric obstruction (gastric volvulus), cirrhosis, among others, represent risk factors for the development of AEN [4],[7].
As is the case for most cases described in the literature, this particular case occurred in an elderly man with multiple comorbidities and with upper gastrointestinal bleeding evidenced by hematemesis and melena. The clinical presentation of AEN ranges from hematemesis and/or melena (accounting for almost 90% of the cases) to an asymptomatic black esophagus [10],[11]. The system review may reveal abdominal pain, vomiting, dysphagia, nausea, fever, vertigo, and syncope. Other associated clinical disorders or endoscopic findings may include multiple organ failure, cardiac, lung and renal disease, DM and ketoacidosis, coagulopathy, peptic ulcer, general weakness and malnutrition, cirrhosis, acute alcoholic hepatitis, acute pancreatitis, sepsis, ischemic processes (stroke, intestinal ischemia), and trauma. Physical findings are generally confused with the underlying medical conditions, but may include cachexia, fever, hypoxia, pallor, and hemodynamic instability, including arrhythmia and hypotension. Laboratory analysis may show leukocytosis and anemia and CT may reveal thickening of the distal esophagus, hiatal hernia, dilated stomach with possible gastric obstruction and, rarely, extrinsic compression of the esophagus by a mediastinal mass [12].
The etiology of this disease is multifactorial and is assumed to be derived from the combination of three factors: esophageal ischemia, reduction of the mucosal barrier systems, and backflow injury from chemical contents of gastric secretions [8]. In this case, although there is no evidence of a clear etiologic cause, we consider an ischemic mechanism in association with base multi-pathology.
The diagnosis of this entity is established by the presence of characteristic endoscopic changes, such as the presence of diffuse dark pigmentation of the esophagus with ulcerations, that corresponds to the severe acute inflammation and mucosal necrosis; circumferential black esophagus, with or without exudates; preferentially distal compromise with proximal extension; well-defined border between the esophageal lesions and the unaffected gastric mucosa [8]. Esophageal tissue biopsy and smear, although not required, contribute and strengthen diagnostic confirmation [12].
Some complications associated with this disease are esophageal stenosis, perforation, and mediastinal abscess.
This patient presented a favorable clinical evolution with conservative treatment. Timely systemic resuscitation and patient stabilization play pivotal roles in the management of this disease. The management of the underlying medical conditions is also imperative. Nil-per-os and intravenous hydration should be established, anemia should be corrected with red blood cell transfusion, acid suppression should be optimized with intravenous proton pump inhibitors, and the treatment of infections or sepsis, when applicable, with appropriate broad spectrum antibiotic. In malnourished patients, parental support may be necessary to improve nutritional status and enhance healing. Early surgical intervention may also be necessary in cases of esophageal perforation and/or mediastinal abscess [13].
Acute esophageal necrosis is not considered a terminal event; not inevitably being a fatal or irreversible situation [14]. The prognosis appears to be more dependent of clinical condition, comorbidities, and advanced age of patients, than esophageal lesions [5],[15].
CONCLUSION
This rare condition appears in a clinical feature characteristic of upper gastrointestinal bleeding. Although it is assumed that the main event is ischemia, in most cases, its etiopathogenesis continues to be unknown, and no cause or unique mechanism is pointed out. Most patients have a base multi-pathology, which seems to restrict the prognosis more than esophageal lesions per se. The importance of an early diagnosis and a targeted treatment to the underlying causes is emphasized, in order to prevent future complications.
REFERENCE
1.
Goldenberg SP, Wain SL, Marignani P. Acute necrotizing esophagitis. Gastroenterology 1990;98(2):493–6. [CrossRef]
[Pubmed]

2.
Cattan P, Cuillerier E, Cellier C, et al. Black esophagus associated with herpes esophagitis. Gastrointest Endosc 1999;49(1):105–7. [CrossRef]
[Pubmed]

3.
Le K, Ahmed A. Acute necrotizing esophagitis: Case report and review of the literature. J La State Med Soc 2007;159(6):330–8.
[Pubmed]

4.
Grudell ABM, Mueller PS, Viggiano TR. Black esophagus: Report of six cases and review of the literature, 1963–2003. Dis Esophagus 2006;19(2):105–10. [CrossRef]
[Pubmed]

5.
Augusto F, Fernandes V, Cremers MI, et al. Acute necrotizing esophagitis: A large retrospective case series. Endoscopy 2004;36(5):411–5. [CrossRef]
[Pubmed]

6.
Lacy BE, Toor A, Bensen SP, Rothstein RI, Maheshwari Y. Acute esophageal necrosis: Report of two cases and a review of the literature. Gastrointest Endosc 1999;49(4 Pt 1):527–32. [CrossRef]
[Pubmed]

7.
Ben Soussan E, Savoye G, Hochain P, et al. Acute esophageal necrosis: A 1-year prospective study. Gastrointest Endosc 2002;56(2):213–7. [CrossRef]
[Pubmed]

8.
Araújo R, Castanheira A, Machado J, et al. Acute necrosis of oesophagus. [Article in Portuguese]. Acta Med Port 2011;24(4):653–6.
[Pubmed]

9.
10.
Gurvits GE, Shapsis A, Lau N, Gualtieri N, Robilotti JG. Acute esophageal necrosis: A rare syndrome. J Gastroenterol 2007;42(1):29–38. [CrossRef]
[Pubmed]

11.
Rejchrt S, Douda T, Kopácová M, et al. Acute esophageal necrosis (black esophagus): Endoscopic and histopathologic appearance. Endoscopy 2004;36(12):1133. [CrossRef]
[Pubmed]

12.
Gurvits GE. Black esophagus: Acute esophageal necrosis syndrome. World J Gastroenterol 2010;16(26):3219–25. [CrossRef]
[Pubmed]

13.
14.
Kram M, Gorenstein L, Eisen D, Cohen D. Acute esophageal necrosis associated with gastric volvulus. Gastrointest Endosc 2000;51(5):610–2. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgement
José Maria Sousa, Centro Hospitalar Universitário de São João – Resident, Neuroradiology Department, Porto, Portugal, sousa.jose99@gmail.com
Telma Fonseca, Centro Hospitalar Universitário de São João – Resident, General Surgery Department, Porto, Portugal, tnvfonseca@gmail.com
Catarina Muller - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ricardo Viveiros - Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Sara Rodrigues - Acquisition of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
António Ferrão - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Elisabete Barbosa - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
José Barbosa - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 Catarina Muller et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.