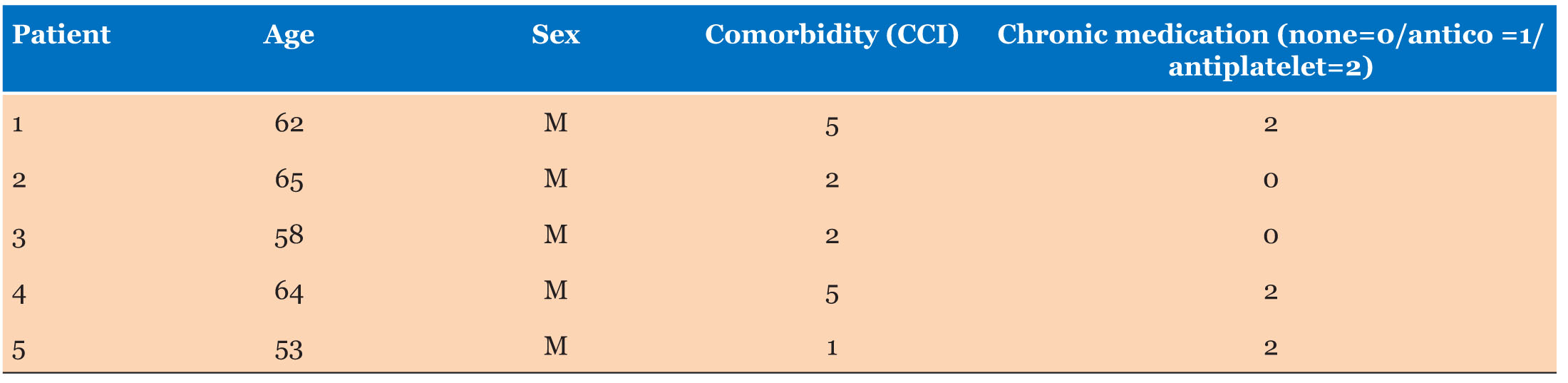
|
Case Series
Purple urine bag syndrome: An unusual presentation of urinary tract infection
1 Senior Physician Specialist, Department of Internal Medicine, Tamale Teaching Hospital, Tamale, Ghana
2 Lecturer, University for Development Studies, School of Medicine and Health Sciences, Tamale, Ghana
Address correspondence to:
Abdul-Subulr Yakubu
Department of Internal Medicine, Tamale Teaching Hospital, Tamale,
Ghana
Message to Corresponding Author
Article ID: 100115Z06AY2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Yakubu AS, Adam A, Ahadzi D. Purple urine bag syndrome: An unusual presentation of urinary tract infection. Case Rep Int 2023;12(1):12–17.ABSTRACT
Introduction: Purple urine bag syndrome is a rare clinical entity characterized by purple discoloration of the urinary catheter and urinary drainage bag in chronically catheterized patients. Though it can be alarming to patients and clinicians, it is considered benign but can indicate an underlying urinary tract infection.
Case Series: The first case was a 68-year-old woman with multiple comorbidities who was admitted to the orthopedic ward with a close fracture of the neck of the right femur. She was bedridden and had an indwelling urethral catheter. Her urine bag was noticed to stain purplish 22 days after bladder catheterization. Urine culture showed a heavy mixed growth. A change of urinary catheter and drainage bag led to a resolution of the condition. The second case was a 58-year-old male who was admitted on account of decompensated liver cirrhosis from chronic hepatitis C virus infection. He also had quadriparesis due to a traumatic cervical spine injury, urine retention, and constipation. On day 24 of his admission, his urine bag was stained with a purplish hue. A urine culture grew Klebsiella oxytoca. The urine bag remained clear and contained amber-colored urine after catheter changes and antibiotic treatment for cystitis.
Conclusion: Purple urine bag syndrome can be alarming to the patient and caregiver who need to be reassured of its benign nature. Urine culture would identify any associated infection. Good catheter care, control of risk factors including constipation and antibiotic treatment for symptomatic urinary tract infection leads to the resolution of the discoloration.
Keywords: Ghana, Indigo, Indirubin, Purple urine
INTRODUCTION
Purple urine bag syndrome (PUBS) is a rare clinical entity characterized by purple discoloration of urinary catheters and drainage bags in chronically catheterized patients [1]. The color is produced by the metabolites of tryptophan, which are found in high levels in the gut of constipated patients [2],[3],[4] . It is considered benign but could be alarming to patients and clinicians and can indicate urinary tract infection (UTI) caused by bacteria containing sulfatase and phosphatase enzymes [5],[6],[7]. We present two cases of PUBS in patients with multiple comorbidities and long-term indwelling urethral catheterization to shed light on this rare entity that can be a source of confusion and baffle the patient, caregivers, and the unsuspecting clinician.
Case Series
Case 1
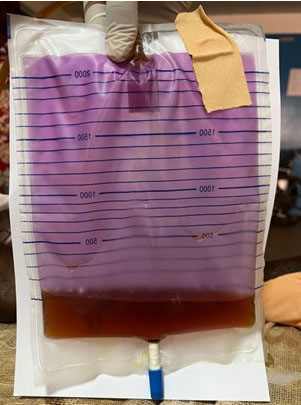
A 68-year-old woman was admitted to the orthopedic ward of Korle Bu Teaching Hospital with a close fracture of the neck of the right femur and had been on admission for eleven weeks. Her past medical history included hypertension, stage IV chronic kidney disease, and hypertensive heart disease. She had been catheterized while on admission (because of mobility constraints) to monitor her fluid balance. Her urine bag was noticed to stain purplish 22 days after bladder catheterization. On physical examination, the patient was afebrile, had conjunctival pallor and her vital signs were within normal limits. Her jugular venous pressure was raised and the cardiac apex was displaced to the sixth intercostal space. Her chest and abdominal examination were unremarkable. Her right leg was shortened and mildly edematous. Purple-colored urine was noted in her urine catheter bag and tubing (Figure 1).
The patient’s urine catheter was changed, and a urine sample was collected into a clean sample container at the time of catheter change through the new catheter and transported immediately to the laboratory. The urine dipstick showed 4+ protein, 1+ blood, and 1+ leucocytes. Glucose, ketones, and nitrite were absent. The urine pH was 8.5 and microscopy showed pus cells of 18 per high power field (HPF), red blood cells of 13/HPF, and epithelial cells of 4/HPF. Triple phosphate (Magnesium ammonium phosphate) crystals were present. There were no casts. Urine culture showed a heavy mixed growth. She was mildly anemic with a hemoglobin level of 10.6 g/dL. The rest of her full blood count indices were within normal limits. Serum creatinine and urea levels were elevated at 319 µmol/L and 11.8 mmol/L respectively. She had an estimated glomerular filtration rate of 16 mL/min/1.73 m2. Serum electrolytes were within normal limits. The rest of her workup included an electrocardiogram that showed left ventricular hypertrophy and a chest X-ray that showed cardiomegaly.
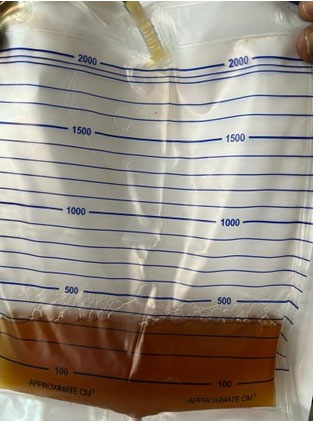
A broad-spectrum antibiotic (intravenous ceftriaxone 2 g daily, which she received for two weeks) was started for a presumed UTI. Fluid balance was carefully maintained. She was also receiving intravenous furosemide and oral bisoprolol 5 mg daily for heart failure. Her other medications included atorvastatin (10 mg daily), soluble aspirin (75 mg daily), oral paracetamol and prophylactic doses of subcutaneous dalteparin. She was also being managed non-surgically by the orthopedic team. There was a gradual clearance of the purple hue from the urine and by the fourteenth week of admission, the purple color had cleared and the urine was uniformly amber (Figure 2). Her clinical course was complicated by a deep vein thrombosis. She made a good recovery and there was an improvement in her urine output from 200 mL to about 1000 mL per day (while on diuretics). Her condition remained stable, and she was discharged home on the 17th of June 2016, after 14 weeks on admission, and scheduled for outpatient reviews.
Case 2
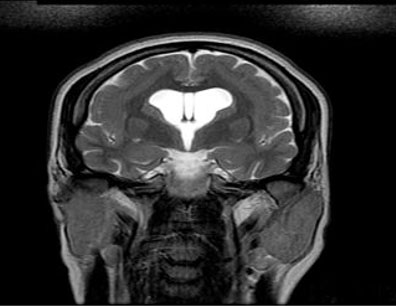
The patient was a 58-year-old male who was admitted to the medical ward of Tamale Teaching Hospital with the diagnosis of decompensated liver cirrhosis from chronic hepatitis C virus infection. He also had quadriparesis due to a traumatic cervical spine injury (following a road traffic accident), urine retention for which he was catheterized, constipation, and decubitus ulcers. His medication included sofosbuvir/velpatasvir, spironolactone, furosemide, rivaroxaban, oral lactulose, doxycycline, cefpodoxime, and multivitamin tablets. On day 24 of his admission, his urine bag (which was in situ since admission) was stained with a purplish hue (Figure 3).
On examination, he was chronically ill-looking and pale. He was anicteric and afebrile but had bilateral pedal edema. He was conscious and alert. He had reduced breath sounds at the lung bases. His respiratory rate was 18 cycles per minute and oxygen saturation was 97% on room air. His blood pressure was 90/63 mmHg and heart sounds were normal. He had mild ascites, and the abdomen was slightly tender in the epigastric and suprapubic regions. A urine culture grew Klebsiella oxytoca which was sensitive to meropenem and amikacin. He was treated with intravenous meropenem for seven days and the urine catheter and bag were changed. The urine bag remained clear and contained amber-colored urine till the patient was discharged home after 32 days of admission (Figure 4).
DISCUSSION
Historically, PUBS is believed to date back to 1812 when King George III was noted to have a bluish discoloration of his urine and the urinary catheter and bag [8]. Since it was first reported in 1978, PUBS has been increasingly reported in patients on long-term urinary catheterization [1]. People with PUBS usually do not complain of any symptoms apart from the discovery of a blue or purple discoloration of the urine which is often a cause for concern to the patient, their caregivers, and the unsuspecting physician. It is generally considered a benign condition, although it may herald the presence of a UTI [9]. Bhattarai et al. reported a case of PUBS in an elderly female who died after vancomycin-resistant Enterococci and Pseudomonas aeruginosa was isolated from her urine, suggesting that it may not always be benign and should be approached on a case-by-case basis to identify those associated with difficult-to-treat UTIs [7].
Women are more frequently affected by PUBS; however, as in our second case, several male cases have been reported [6],[10]. Purple urine bag syndrome is associated with UTI caused by bacteria that produce sulfatase or phosphatase enzymes [2]. Female gender, constipation, UTI (especially with a high urinary bacterial count), alkaline urine, and dementia are associated with PUBS [7],[8]. As in the two cases presented, almost all patients with purple urine bag syndrome are catheterized due to significant disability. Constipation is believed to promote bacterial metabolism of tryptophan to indole, resulting in high levels of indigo and indirubin in the urine [4]. Purple urine bag syndrome has been reported in patients with acidic urine [11].
Both cases presented had the typical characteristics of the patient with PUBS: elderly with multiple comorbidities and long-term indwelling urinary catheterization. The heavy bacterial load and alkaline urine in the first case are additional factors that favored the development of the condition. The response to catheter changes and antibiotics for symptomatic UTI (second case) was also typical of PUBS. A prevalence of PUBS as high as 9.9% was reported in institutionalized women with long-term indwelling urinary catheters [3].
The purple color is due to the compounds indigo and indirubin, which are metabolic degradation products of tryptophan [2],[6]. The pathogenesis is believed to begin with the conversion of dietary tryptophan to indole by gut bacteria. This undergoes liver metabolism to indoxyl sulfate which is then excreted in the urine. In the urine, indoxyl sulfate can be converted by bacteria colonizing the urinary catheter to indoxyl, which is further converted to indigo (blue) and indirubin (red) [2]. These pigments result in a deep purple color after interaction with the plastic tubing. The bacteria most commonly associated with PUBS are Escherichia coli, Klebsiella pneumonia, Provedencia species, Pseudomonas aeruginosa, Proteus mirabilis, Enterococcus species, Streptococcus species, and Staphylococcus species [2],[5],[12],[13],[14].
Generally, there is no specific recommended approach for diagnosing PUBS [15]. Visual identification of the purple urine in bag and tubing and simple microbiology (urinalysis, urine culture) and biochemistry tests usually suffice. Purple urine bag syndrome is a sign of colonization of the urinary catheter system; hence, antibiotic therapy may only be indicated in patients with symptomatic UTI and is not recommended for asymptomatic bacteriuria [16]. For asymptomatic patients, treatment of underlying risk factors (including control of constipation) and good catheter care usually suffice [12],[16]. Even though both of our cases were treated with antibiotics, merely changing the catheters and drainage bags might have sufficed. The presence of suprapubic tenderness suggestive of cystitis might have justified the use of antibiotics in the second case. The mainstay of preventing purple urine bag syndrome is regular changing of indwelling catheters and ensuring prompt removal of urinary catheters once they are no longer needed. The clinical need for bladder catheterization needs to be reviewed regularly and the catheter removed as soon as possible. Adequate fluid intake, catheter hygiene and avoidance of constipation are essential parts of catheter care best practice [16]. The cases presented highlight the importance of proper care of indwelling urethral catheters and the need to have and adhere to institutional protocols for proper care of urinary catheters.
CONCLUSION
We presented two cases of PUBS in hospitalized patients with multiple comorbidities and long-term indwelling urethral catheters. Purple urine bag syndrome can be diagnosed by visual identification of purple discoloration of the urinary bag and catheter tubing. It can be alarming to the patient and caregiver who need to be reassured of its benign nature. The management of PUBS is directed at good catheter care and control of risk factors including constipation. Antibiotic treatment is recommended for underlying symptomatic UTI.
REFERENCE
1.
Barlow GB, Dickson JAS. Purple urine bags. Lancet 1978;311:220–1. [CrossRef]

2.
Dealler SF, Hawkey PM, Millar MR. Enzymatic degradation of urinary indoxyl sulfate by Providencia stuartii and Klebsiella pneumoniae causes the purple urine bag syndrome. J Clin Microbiol 1988;26(10):2152–6. [CrossRef]
[Pubmed]

3.
Dealler SF, Belfield PW, Bedford M, Whitley AJ, Mulley GP. Purple urine bags. J Urol 1989;142(3):769–70. [CrossRef]
[Pubmed]

4.
Ga H, Kojima T. Purple urine bag syndrome. JAMA 2012;307(18):1912–3. [CrossRef]
[Pubmed]

5.
Khan F, Chaudhry MA, Qureshi N, Cowley B. Purple urine bag syndrome: An alarming hue? A brief review of the literature. Int J Nephrol 2011;2011:419213. [CrossRef]
[Pubmed]

6.
Hadano Y, Shimizu T, Takada S, Inoue T, Sorano S. An update on purple urine bag syndrome. Int J Gen Med 2012;5:707–10. [CrossRef]
[Pubmed]

7.
Bhattarai M, Bin Mukhtar H, Davis TW, Silodia A, Nepal H. Purple urine bag syndrome may not be benign: A case report and brief review of the literature. Case Rep Infect Dis 2013;2013:863853. [CrossRef]
[Pubmed]

8.
Arnold WN. King George III’s urine and indigo blue. Lancet 1996;347(9018):1811–3. [CrossRef]
[Pubmed]

9.
Lin J, Hlafka M, Vargas O, Bhattarai M. Recurrent purple urine bag syndrome presenting with full spectrum of disease severity: Case report and review of literature. CEN Case Rep 2016;5(2):144–7. [CrossRef]
[Pubmed]

10.
Van Keer J, Detroyer D, Bammens B. Purple urine bag syndrome in two elderly men with urinary tract infection. Case Rep Nephrol 2015;2015:746981. [CrossRef]
[Pubmed]

11.
Chung SD, Liao CH, Sun HD. Purple urine bag syndrome with acidic urine. Int J Infect Dis 2008;12(5):526–7. [CrossRef]
[Pubmed]

12.
Lin CH, Huang HT, Chien CC, Tzeng DS, Lung FW. Purple urine bag syndrome in nursing homes: Ten elderly case reports and a literature review. Clin Interv Aging 2008;3(4):729–34. [CrossRef]
[Pubmed]

13.
Su FH, Chung SY, Chen MH, et al. Case analysis of purple urine-bag syndrome at a long-term care service in a community hospital. Chang Gung Med J 2005;28(9):636–42.
[Pubmed]

14.
Yaqub S, Mohkum S, Mukhtar KN. Purple urine bag syndrome: A case report and review of literature. Indian J Nephrol 2013;23(2):140–2. [CrossRef]
[Pubmed]

15.
16.
Reid S, Brocksom J, Hamid R, et al. British Association of Urological Surgeons (BAUS) and Nurses (BAUN) consensus document: Management of the complications of long-term indwelling catheters. BJU Int 2021;128(6):667–77. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgement
We wish to thank Dr. Rashid Konney for his role in the care of the patient as well as the acquisition of data.
Author ContributionsAbdul-Subulr Yakubu - Conception of the work, Design of the work, Acquisition of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Atiku Adam - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Dzifa Ahadzi - Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2023 Abdul-Subulr Yakubu et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.