|
Case Report
Late occurrence of ChAdOx1 vaccine-induced myocarditis presenting with ventricular arrhythmia
1 MBBS, MD, DM, Director Cardiology, Supreme Hospital, Delhi NCR, India
Address correspondence to:
Deepak Natarajan
MBBS, MD, DM, Director Cardiology, Supreme Hospital, Delhi NCR,
India
Message to Corresponding Author
Article ID: 100116Z06DN2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Natarajan D, Rana P. Late occurrence of ChAdOx1 vaccine-induced myocarditis presenting with ventricular arrhythmia. Case Rep Int 2023;12(1):18–22.ABSTRACT
A 51-year-old woman who had received 2 injections of a ChAdOx1 vaccine in 2021 and a booster dose in 2022 was recently admitted for central chest pain accompanied with palpitations for the previous 2 weeks. She was negative for the COVID-19 virus, troponin was not elevated, both the 12-lead electrocardiogram and 2D echocardiogram were normal. At peak exercise during exercise treadmill test she developed a single ventricular couplet, but coronary angiography revealed normal coronary arteries. A 24-hour electrocardiogram recording revealed symptomatic non-sustained ventricular tachycardia while she was in bed. A 3T cardiac magnetic resonance imaging (MRI) demonstrated late gadolinium sub-epicardial uptake at the left ventricle apex suggesting fibrosis. The patient was diagnosed as late presentation of myocarditis following ChAdOx1 vaccination, and was discharged on oral amiodarone and colchicine.
Keywords: Adenoviral vector vaccine, Cardiac MRI, COVID vaccine myocarditis, Myocarditis, Non-sustained ventricular tachycardia, SARS-CoV-2
INTRODUCTION
India began its severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccine roll out in January 2021, with healthcare workers and frontline workers being the first recipients, followed by those more than 50 years and then those under 50 years with co-morbidities. In one year India delivered 1.57 billion doses according to the WHO. A vaccine programme for 15- to 18-year-olds began in January and for 12- to 14-year-olds in March of 2022. Vaccines against SARS-CoV-2 included the Astra Zeneca adenoviral vector ChAdOx1 (Covishield) and the inactivated BBV152 (COVAXIN) vaccines. The mRNA vaccines, however, have not so far been used in India [1],[2].
The Astra Zeneca ChAdOx1 vaccine uses a chimpanzee adenovirus and encodes the full-length spike protein. It elicits a robust antibody as well as a T-cell response.
The ChAdOx1 vaccine delivers the genetic code in a double-stranded DNA into the nucleus to manufacture spike proteins [3].
Most European nations suspended use of the ChAdOx1 vaccine due to association of serious adverse effects such as thrombotic thrombocytopenia and Guillain–Barre disease beginning March 2021 [4].
Soon multiple reports of increased risk of myocarditis associated with the mRNA vaccine were published, with the incidence of mRNA vaccine-related myocarditis usually occurring in young males (12–29 years) after the second dose. Importantly, markedly raised levels of free spike proteins unbound by antibodies have been observed in adolescents with post-mRNA vaccine-induced myocarditis [5],[6],[7].
Autopsy reports confirming myocarditis have suggested either an autoimmune mechanism or direct toxicity by the spike protein produced by mRNA vaccine. The presence of spike protein in the absence of the nucleocapsid protein in an inflamed tissue is confirmation that the spike protein is the result of the vaccine and not because of infection by SARS-CoV-2 [7].
Markedly raised levels of free spike proteins unbound by antibodies have been observed in adolescents with post-mRNA vaccine myocarditis [8].
This report describes a triple ChAdOx1 vaccine inoculated Indian woman presenting with apprehension and chest pain accompanied by non-sustained ventricular tachycardia in the presence of normal coronary arteries. There are very few reports of myocarditis associated with the adenoviral vector or ChAdOx1 vaccine, most probably due to early suspension of this vaccine in most parts of the world, and little or no usage in the United States, where the mRNA vaccine has been predominantly employed [9],[10],[11]. Moreover, long-term ramifications of vaccine-induced myocarditis are unknown.
CASE REPORT
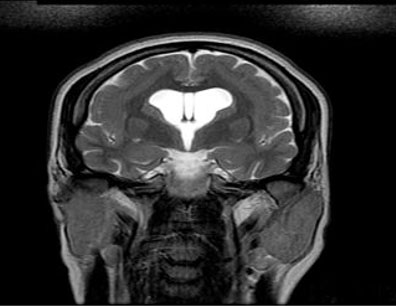
A 51-year-old woman who had received 2 injections of an ChAdOx1 vaccine in 2021 and a booster dose in 2022 was admitted for central chest pain and palpitation for the previous 2 weeks. She also suffered from great apprehension when she felt the palpitations. There was no history of a running nose, sore throat, fever, cough, or breathless in the recent or remote past. A nasopharyngeal viral panel was negative for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), enterovirus, adenovirus, or influenza A and B viruses. She was negative for the human immunodeficiency virus, hepatitis B and hepatitis C viruses. The 12-lead electrocardiogram was normal, while the 2D Doppler echocardiogram was unremarkable for wall motion abnormality, valvulopathy, or pericardial pathology. Troponin was not raised. An exercise treadmill test was negative for ischemia but a ventricular couplet was recorded at peak exercise (Figure 1). The patient underwent coronary angiography that revealed normal left and right coronary arteries (Figure 2). A 24-hour electrocardiogram recording revealed a short run of non-sustained ventricular tachycardia (NSVT) at heart rate of 110 per minute late at night while she was awake but in bed (Figure 3). She felt both chest pain and was apprehensive during this episode. Cardiac T3 MRI showed a late gadolinium sub-epicardial enhancement in the left ventricular apex (Figure 4) with normal left ventricle function. A provisional diagnosis of vaccine-induced late myocarditis scar was made and the patient discharged on tablet amiodarone subsequent to a loading bolus injection, and tablet colchicine 0.5 mg twice a day. At one month follow-up, the patient is asymptomatic without ventricular ectopy.
DISCUSSION
This report describes a 51-year-old woman who was twice vaccinated and boosted more than a year ago and presented with non-sustained ventricular tachycardia, normal coronary arteries, and intra-myocardial scar tissue in the apex as assessed by late gadolinium cardiac magnetic resonance imaging (CMRI). Myocarditis following vaccination is an established fact, with the incidence being greater than infection with SARS-CoV-2 or the background rate.
A large Nordic study including 23 million people concluded that risk of myocarditis and pericarditis was increased post-mRNA vaccination. Risk was highest in young males (16–24 years) after the second dose [12].
A meta-analysis including 29 studies from across the world found the highest incidence of vaccine-induced myocarditis ranged from 81 to 390 per million per persons (doses). The meta-analysis includes six studies reporting an incidence greater than 150 cases per million persons (doses) in males aged 12–24 years after 2 doses of mRNA vaccine. This meta-analysis shows higher rates of myocarditis than reported by the CDC (Vaccine Adverse Events Reporting System) that had documented 46 cases per million doses in those aged 12–15 years and 76 per million doses in those aged 16–17 years. The risk of myocarditis increases after the second dose in those under 25 years of age [13].
Rates of post-vaccination myocarditis is reliable because both the number of doses administered and cases of myocarditis are known. However, the probability of subclinical myocarditis that goes unreported needs to be factored in any calculation; the incidence rates of vaccine-induced myocarditis are therefore an underestimate. The reverse is true in the case of SARS-CoV-2-induced myocarditis where the denominator is most certainly a fraction of the cases that are infected but not picked up by any surveillance system.
A prospective cohort study from Thailand in 301 young children (aged 13–18 years) has reported 7 cases of myo-pericarditis providing an incidence estimate of 2.3% or 23,000 cases per million persons. One patient had confirmed myocarditis, 2 had suspected pericarditis, and 4 had suspected subclinical myocarditis. Myocarditis was diagnosed on basis of symptoms, ECG changes, 2 D echocardiography and cardiac MRI. The children presented with chest pain, palpitations, and shortness of breath; all had received an mRNA vaccine. The best diagnostic tool to confirm myocarditis by the authors of this study is cardiac MRI [14].
Severe myocarditis resulting in cariogenic shock is also well described albeit not highlighted in literature [15].
Data on adenovirus vector vaccine-induced myocarditis are however sparse. The reason may be that in most Western countries use of adenovector virus vaccine was terminated in March 2021 itself because of cases of vaccine-induced thrombotic thrombocytopenia (VITT). Reports of 39 persons who were previously healthy with no preexisting prothrombotic condition developing a newly described syndrome of thrombosis accompanied by thrombocytopenia 5–24 days after vaccination with the ChAdOx1 nCoV-19 vaccine were published in 2021. Thrombosis was found in unusual sites, such as the hepatic or portal veins, apart from the cerebral venous sinuses. Median platelet count, in these patients, at diagnosis was 20,000–30,000 mm3, with high levels of D-dimer, and high levels of antibodies to platelet factor 4 (PF4). The pathogenesis for VITT is believed to be molecular mimicry of some component of the spike protein or the adenoviral vector vaccine with platelet factor 4 [9],[10],[11].
A 33-year-old male has been reported to develop symptoms of myocarditis as soon as two days after a single dose of the Janssen Ad26 COV-2 S vaccine. The patient presented with chest pain, rise in troponin, and focal myocarditis detected by cardiac MRI. The patient was discharged home in stable condition with close follow-up [16].
There is a rare case report of a 28-year-old male presenting five days after an adenovirus vector vaccination with chest pain at rest but no fever or cough. His chest X-ray was normal, the electrocardiogram (ECG) showed 1 mm ST segment elevation leads II, V5–V6, mild global hypokinesia on 2D echocardiography, and no obstruction in his coronary arteries. There was a patchy mid-subepicardial late gadolinium enhancement throughout the mid to apical left ventricular wall but no edema or pericardial involvement. The cardiac MRI was done 37 days post-vaccination. The patient was hospitalized for two days only [17].
A Spanish report describes severe myocarditis in a 68-year-old male following first dose of adenovirus vector vaccination 37 days earlier. The ECG suggested an acute myocardial infarction but coronary angiography done revealed normal coronary arteries. Cardiac MRI confirmed myocarditis, with the patient requiring inotropic and vasopressor support [7].
An Iranian report describes a 32-year-old female developing myocarditis after the first dose of an adenovirus vector vaccine. The patient developed exertion tachycardia and breathlessness three days post-vaccination, but a diagnosis of myocarditis was made much later at three months by 2D echocardiography. There was no confirmation of association between vaccination and myocarditis [18].
There is endo-myocardial biopsy confirmation of 2 patients developing myocarditis within a fortnight of vaccination with the ChAdOx1 vaccine; the patients presented with depressed left ventricle function as assessed by 2D echocardiogram. There were two cases of post-adenovirus vector Janssen myocarditis in this series, along with 11 cases of myocarditis following mRNA vaccination [19].
Apart from molecular mimicry between some component of the ChAdOx1 vaccine and cardiac tissue, there is also the possibility of contaminants in the commercially prepared adenovirus vector vaccine. ChAdOx1vccine has been found to have significantly higher than expected levels of host cell proteins (HCPs) and free viral proteins. The most abundant contaminating HCPs are the heat shock protein and cytoskeleton protein families. The role of these impurities in triggering cardiac inflammation remains to be determined [20].
The question of any long-term consequences of vaccine-associated myocarditis persists, making long-term follow-up of these patients mandatory. The biological mechanism linking COVID-19 mRNA or adenovirus vector vaccination to rare cases of acute myocarditis and pericarditis also remain to be answered.
The clinical presentations of Myocarditis after COVID-19 mRNA vaccination have been predominantly mild and few patients have required intensive treatment.
CONCLUSION
This case report describes the late presentation of ChAdOx1 vaccine-induced myocarditis in a middle-aged woman who underwent two inoculations in 2021 and a booster in 2022. Even though a causeand-effect relationship between the vaccine and the resulting myocarditis cannot be proven, the presence of subepicardial scar tissue in the apex of a normally functioning left ventricle on cardiac MRI strongly suggests a previous subclinical myocarditis after vaccination. Crucially, it cannot be overemphasised that the appearance of a ventricular couplet at peak exercise during an exercise treadmill test may be a marker for sudden death.
REFERENCE
1.
Desai D, Khan AR, Soneja M, et al. Effectiveness of an inactivated virus-based SARS-CoV-2 vaccine, BBV152, in India: A test-negative, case-control study. Lancet Infect Dis 2022;22(3):349–56. [CrossRef]
[Pubmed]

2.
Ella R, Reddy S, Jogdand H, et al. Safety and immunogenicity of an inactivated SARS-CoV-2 vaccine, BBV152: Interim results from a double-blind, randomised, multicentre, phase 2 trial, and 3-month follow-up of a double-blind, randomised phase 1 trial. Lancet Infect Dis 2021;21(7):950–61. [CrossRef]
[Pubmed]

3.
Voysey M, Clemens SAC, Madhi SA, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: An interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 2021;397(10269):99–111. [CrossRef]
[Pubmed]

4.
Wise J. Covid-19: European countries suspend use of Oxford-AstraZeneca vaccine after reports of blood clots. BMJ 2021;372:n699. [CrossRef]
[Pubmed]

5.
6.
Turni C, Lefringhausen A. COVID 19 vaccines – An Australian review. J Clin Exp Immunol 2022;7(3):491–508. [CrossRef]

7.
Mörz M. A case report: Multifocal necrotizing encephalitis and myocarditis after BNT162b2 mRNA vaccination against COVID-19. Vaccines (Basel) 2022;10(10):1651. [CrossRef]
[Pubmed]

8.
Yonker LM, Swank Z, Bartsch YC, et al. Circulating spike protein detected in post-COVID-19 mRNA vaccine myocarditis. Circulation 2023;147(11):867–76. [CrossRef]
[Pubmed]

9.
Cines DB, Bussel JB. SARS-CoV-2 vaccine-induced immune thrombotic thrombocytopenia. N Engl J Med 2021;384(23):2254–6. [CrossRef]
[Pubmed]

10.
Greinacher A, Thiele T, Warkentin TE, et al. Thrombotic thrombocytopenia after ChAdOx1 nCov-19 vaccination. N Engl J Med 2021;384(22):2092– 101. [CrossRef]
[Pubmed]

11.
Schultz NH, Sørvoll IH, Michelsen AE, et al. Thrombosis and thrombocytopenia after ChAdOx1 nCoV-19 vaccination. N Engl J Med 2021;384(22):2124–30. [CrossRef]
[Pubmed]

12.
Karistad Ø, Hovi P, Husby A, et al. SARS-CoV-2 vaccination and myocarditis in a Nordic cohort study of 23 million residents. JAMA Cardiol 2022;7(6):600–12. [CrossRef]
[Pubmed]

13.
Knudsen B, Prasad V. COVID-19 vaccine induced myocarditis in young males: A systematic review. Eur J Clin Invest 2022;53(4):e13947. [CrossRef]
[Pubmed]

14.
Mansanguan S, Charunwatthana P, Piyaphanee W, et al. Cardiovascular manifestation of the BNT162b2 mRNA COVID-19 vaccine in adolescents. Trop Med Infect Dis 2022;7(8):196. [CrossRef]
[Pubmed]

15.
Verma AK, Lavine KJ, Lin CY. Myocarditis after Covid-19 mRNA vaccination. N Engl J Med 2021;385(14):1332–4. [CrossRef]
[Pubmed]

16.
Sulemankhil I, Abdelrahman M, Negi SI. Temporal association between the COVID-19 Ad26.COV2.S vaccine and acute myocarditis: A case report and literature review. Cardiovasc Revasc Med 2022;38:117–23. [CrossRef]
[Pubmed]

17.
Rodríguez RM, Herraiz ATI, González MJG. Cardiogenic shock due to acute myocarditis following AZD122 vaccine administration: A case report. [CrossRef]

18.
Hassanzadeh S, Sadeghi S, Mirdamadi A, Nematollahi A. Myocarditis following AstraZeneca (an adenovirus vector vaccine) COVID-19 vaccination: A case report. Clin Case Rep 2022;10(4):e05744. [CrossRef]
[Pubmed]

19.
Baumeier C, Aleshcheva G, Harms D, et al. Intramyocardial inflammation after COVID-19 vaccination: An endomyocardial biopsy-proven case series. Int J Mol Sci 2022;23(13):6940. [CrossRef]
[Pubmed]

20.
Krutzke L, Rösler R, Allmendinger E, Engler T, Wiese S, Kochanek S. Process- and product-related impurities in the ChAdOx1 nCov-19 vaccine. Elife 2022;11:e78513. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Deepak Natarajan - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Poonam Rana - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2023 Deepak Natarajan et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.