|
Case Report
Lupus mastitis: Suspicious breast lesion as a rare presentation of lupus
1 Resident, General Surgery Department, Hospital do Espírito Santo de Évora, Évora, Portugal
2 Surgeon, General Surgery Department, Hospital do Espírito Santo de Évora, Évora, Portugal
3 Senior Surgeon, General Surgery Department, Hospital do Espírito Santo de Évora, Évora, Portugal
4 Retired Senior Surgeon, Former Chief of Department, General Surgery Department, Hospital do Espírito Santo de Évora, Évora, Portugal
5 Chief of Department, General Surgery Department, Hospital do Espírito Santo de Évora, Évora, Portugal
Address correspondence to:
Maria Cristina Botelho Hasse Velez
R. Almada Negreiros, 28, 7005-288 Évora,
Portugal
Message to Corresponding Author
Article ID: 100118Z06MV2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Velez MCBH, Lima R, Ribeiro S, Félix R, Caravana J, Carvalho M. Lupus mastitis: Suspicious breast lesion as a rare presentation of lupus. Case Rep Int 2023;12(2):1–5.ABSTRACT
Introduction: Lupus mastitis is a rare disease. Rarely it can present in a patient without the diagnosis of lupus, being its first and even only manifestation. This makes the diagnosis even more challenging. The authors present a case that shows the difficult clinical pathway from diagnosis to treatment of an infrequent and poorly known disease.
Case Report: A 42-year-old female was referred to our breast surgery outpatient clinic for a suspicious lesion in her right breast with a 10-month evolution. The patient had already been submitted to a series of imaging procedures and tissue biopsies. She did not have history of any autoimmune diseases. The patient was evaluated by different specialties and the diagnosis of lupus mastitis posed a challenge for all physicians involved. Since both clinicians and patient were concerned with malignancy, an excisional biopsy was performed. Lupus mastitis was the definitive diagnosis. The postoperative healing was challenging. The question whether excisional biopsy should or not be performed, as well as surgical procedures in general, was brought up. The risk and fear of malignancy were weighted against the gain of the procedure.
Conclusion: Lupus mastitis is a rare and likely overlooked disease. It should be taken into consideration as a differential diagnosis for suspicious breast lesions. Need for surgery, being it excisional biopsy or lumpectomy, should be carefully weighted. This decision should be based on the risk of malignancy and efficacy of medical treatment.
Keywords: Autoimmune disease, Breast suspicious lesion, Challenging diagnosis, Lupus mastitis
INTRODUCTION
Lupus mastitis is a rare disease, with less than 50 cases reported to date in the literature [1],[2],[3],[4],[5]. Rarely it can present in a patient without the diagnosis of lupus, being it’s first and even only manifestation [2],[5]. In these cases, the diagnosis is even more challenging and likely to be initially overlooked. Differential diagnosis should include inflammatory breast carcinoma, granulomatous mastitis, and lymphoma. We present a case where the patient had already been submitted to a series of imaging examinations and tissue biopsies with no diagnostic conclusion. Malignancy was an important concern for everyone involved. Having no previous history of systemic lupus erythematosus (SLE) was a relevant factor in deciding for the excisional biopsy. This case shows the difficult clinical pathway from diagnosis to treatment of an infrequent and poorly known disease.
CASE REPORT
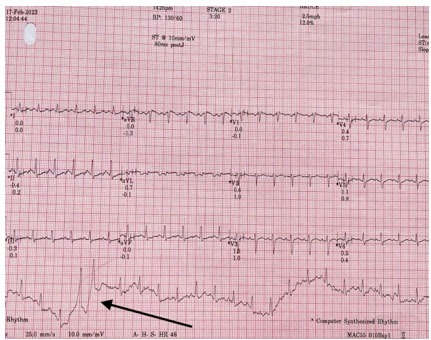
A 42-year-old female with no relevant medical history presented to our General Surgery outpatient clinic. She complained of a palpable right breast lump for the previous ten months and skin alterations with six months of evolution (Figure 1). She had already been observed by breast surgeons in two different hospitals. A breast ultrasound was initially performed that showed a well-defined isoechoic solid lesion with 16×6 mm. A mammogram showed a higher stromal density in the central portion of the right breast and no microcalcifications, pointing to an inflammatory nature (Figure 2). An ultrasound-guided core biopsy was performed that showed no neoplastic cells. Magnetic resonance imaging (MRI) was consistent with an inflammatory process and classified as Breast Image Reporting and Data System (BI-RADS) 3/2. Five months later the diagnosis remained a challenge and a new MRI was performed that showed subacute inflammatory changes (Figure 2). Because of the duration of the alterations, a core biopsy was suggested and it was classified as BI-RADS 3/4a. Meanwhile the patient was referred to a dermatologist, who posed the hypothesis of an autoimmune disease and performed a skin biopsy which showed no neoplastic cells. It was by this time that the patient was referred to our breast surgery outpatient clinic. Since there was no clear diagnosis, another ultrasound-guided core biopsy was requested which showed periductitis and stromal fibrosis. Again no neoplastic tissue was found and no diagnosis was reached. Blood tests performed were normal with the exception of thrombocytopenia with 82,000 platelets per microliter of blood. By this time the patient had a history of a breast lump with associated skin changes for the last year and half, with no signs of getting better. She had been subjected to multiple examinations and cancer was a constant concern. After discussion in a multidisciplinary meeting, an excisional biopsy was proposed to the patient, with which she agreed.
An excisional biopsy was performed using an oncoplastic round block surgical technique (Figure 3). Anatomopathological examination of the excisional biopsy showed an epidermis with no particularities, dermis with lesions of thrombotic vasculitis with occlusion of small- and medium-sized vessels with fibrin. In the surrounding glandular tissue there was fibrosis and an extensive periductal and perilobular lymphocytic inflammatory infiltration with a nodular pattern and some germinative centers, without nuclear atypia. There were also seen foci of hyaline necrosis in the adipose tissue, microcalcifications, and lymphocytic vasculitis. These alterations suggested a lymphocytic mastitis compatible with lupus mastitis. With this pathology result, the patient was then referred to a rheumatologist. Serology for lupus was performed which was positive. Pharmacological therapeutic aiming lupus was initiated with aceclofenac, calciferol, prednisolone, hydroxychloroquine, and colchicine.
Six days after the excisional biopsy the surgical wound started to show signs of poor healing with darkening of the wound edges, which eventually lead to necrosis of two thirds of the nipple areolar complex (Figure 4). Debridement was performed and wound dressing with honey and alginate methylcellulose hydrogel was kept for about two weeks. A month and half after the surgery the wound had completely healed but a significant deformity of the nipple-areolar complex resulted. Despite this, the breast kept it’s natural and previous shape, maintaining a good symmetry with the contralateral breast (Figure 5). Four years after the surgical procedure and beginning of pharmacological therapeutic treatment the patient remains asymptomatic.
DISCUSSION
Lupus is a disease characterized by chronic inflammation of autoimmune origin. It is called discoid lupus erythematosus when only the skin is involved. Lupus panniculitis occurs in 2–3% of patients with systemic or discoid lupus erythematosus. When involving the breast it is called lupus mastitis, being it more common with discoid lupus erythematosus [2],[4],[5],[6],[7],[8]. Histopathological criteria for the diagnosis of lupus mastitis are defined, four major and four minor criteria, without the need of the presence of them all to achieve a diagnosis. Lymphocytic infiltration, periseptal and perilobular panniculitis, hyaline fat necrosis, and microcalcifications are characteristic findings of this disease [1],[4],[5],[7],[9],[10]. In this case, the first diagnosis that was thought of and the authors urged to exclude was inflammatory breast cancer, being oncological disease the main differential diagnosis because of its prognostic relevance. Consequently, tissue sampling is required, usually by core biopsy. Granulomatous mastitis and lymphoma also constitute differential diagnosis of lupus mastitis [2],[4],[11],[12]. Even though previous core biopsies didn’t show cellular atypia, the patient had skin alterations such as erythema and edema, and in some inflammatory breast cancers atypia is not found on core biopsies. In the light of the actual knowledge on this rare disease, surgical procedures are not yet consensual for lupus mastitis, so, we must emphasize that our patient had no previous lupus diagnosis, which made the breast disease even more difficult to diagnose [3],[13]. Despite this, the short number of reported cases where patients with lupus mastitis have been submitted to surgical procedures is not enough to draw conclusions on this matter. Pharmacological treatment aimed at the underlying disease is effective, with steroids and antimalarial drugs, calling into attention the relevance of having a specific diagnosis [1],[3],[4],[7],[9],[13]. The wound complications were undoubtedly a physical and psychological burden for our patient and a concern for the surgical team. Despite this, after complete healing the result is aesthetically acceptable for the patient. A lupus mastitis diagnosis makes these complications understandable, since the microvascular changes certainly played a role in the skin healing process, impeding a normal scarring. Lupus mastitis is a rare disease and this patient had come a long way until getting to our outpatient clinic, with breast changes with more than a year and half of duration. She had a significant concern toward the possibility of having breast cancer. So, in this case, the question whether the excisional biopsy would have been proposed even in the suspicion of the diagnosis is valid, since our pathologists, as most of them don’t have much experience with this diagnosis [14].
CONCLUSION
Lupus mastitis is a rare but likely overlooked disease. This pathology should be posed as a differential diagnosis for breast lumps with skin changes, especially when the patient has a diagnosis of lupus, but not only. Need for surgery, being it excisional biopsy or lumpectomy, should be carefully weighted based on the risk of malignancy and efficacy of medical treatment.
REFERENCE
1.
Warne RR, Taylor D, Segal A, Irish A. Lupus mastitis: A mimicker of breast carcinoma. BMJ Case Rep 2011;2011:bcr1120115066. [CrossRef]
[Pubmed]

2.
Voizard B, Lalonde L, Sanchez LM, et al. Lupus mastitis as a first manifestation of systemic disease: About two cases with a review of the literature. Eur J Radiol 2017;92:124–31. [CrossRef]
[Pubmed]

3.
Bayar S, Dusunceli E, Ceyhan K, Unal E, Turgay M. Lupus mastitis is not a surgical disease. Breast J 2007;13(2):187–8. [CrossRef]
[Pubmed]

4.
Rosa M, Mohammadi A. Lupus mastitis: A review. Ann Diagn Pathol 2013;17(2):230–3. [CrossRef]
[Pubmed]

5.
Thapa A, Parakh A, Arora J, Goel RK. Lupus mastitis of the male breast. BJR Case Rep 2016;2(2):20150290. [CrossRef]
[Pubmed]

6.
Martella S, Matthes AGZ, Bassi F, et al. Lupus mastitis in male mimicking a breast lump. Int J Surg 2008;6(6):e67–9. [CrossRef]
[Pubmed]

7.
Wani AM, Mohd Hussain W, Fatani MI, Shakour BA. Lupus mastitis – Peculiar radiological and pathological features. Indian J Radiol Imaging 2009;19(2):170–2. [CrossRef]
[Pubmed]

8.
Pimentel A, Moreira A, Silva S, Lages R, Noronha J. Lupus mastitis: A rare breast cancer differential diagnosis. Clin Case Rep 2021;9(7):e04416. [CrossRef]
[Pubmed]

9.
Bica BE, Saldarriaga LMR, Rocha ACP. PReS-FINAL-2286: Mastitis in an adolescent patient with juvenile systemic lupus erythematous. Pediatr Rheumatol 2013:11(Suppl 2):P276. [CrossRef]

10.
Lucivero G, Romano C, Ferraraccio F, et al. Lupus mastitis in systemic lupus erythematosus: A rare condition requiring a minimally invasive diagnostic approach. Int J Immunopathol Pharmacol 2011;24(4):1125–9. [CrossRef]
[Pubmed]

11.
Robinson A, Herrmann S, Sadruddin S, et al. Lupus: The great pretender, breast manifestations of SLE. Intl J Cancer Oncol 2015:2(3):1–3. [CrossRef]

12.
Kinonen C, Gattuso P, Reddy VB. Lupus mastitis: An uncommon complication of systemic or discoid lupus. Am J Surg Pathol 2010;34(6):901–6. [CrossRef]
[Pubmed]

13.
Dandinoglu T, Dandin O, Akpak YK, Ergin T, Karadeniz M. Can lupus mastitis be treated surgically? Orthop Muscul Syst 2014;3:1000151. [CrossRef]

14.
Georgian-Smith D, Lawton TJ, Moe RE, Couser WG. Lupus mastitis: Radiologic and pathologic features. AJR Am J Roentgenol 2002;178(5):1233–5. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Maria Cristina Botelho Hasse Velez - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Rita Lima - Acquisition of data, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Susana Ribeiro - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Rosa Félix - Conception of the work, Design of the work, Analysis of data, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Jorge Caravana - Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Manuel Carvalho - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2023 Maria Cristina Botelho Hasse Velez et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.