|
Case Report
Mediastinal dumbbell hydatid cyst compressing the thoracic spinal cord: A case report and literature review
1 Assistant Professor of Neurosurgery, Department of Neurosurgery, St. Paul’s Millennium Medical College, Addis Ababa, Ethiopia
2 Senior Neurosurgical Resident, Department of Neurosurgery, St. Paul’s Millennium Medical College, Addis Ababa, Ethiopia
3 Associate Professor of Neurosurgery, University of Texas at San Antonio, San Antonio, TX, USA
Address correspondence to:
Abraham Tadele
Addis Ababa,
Ethiopia
Message to Corresponding Author
Article ID: 100125Z06AT2024
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Tadele A, Hussen E, Gebreegziabher B, Mesfin F. Mediastinal dumbbell hydatid cyst compressing the thoracic spinal cord: A case report and literature review. Case Rep Int 2023;12(1):30–35.ABSTRACT
Introduction: Hydatid disease, or echinococcosis, is a parasitic infection of humans caused by tapeworms of the genus Echinococcus. The liver and lungs are the most common organs to be involved. Mediastinal and bone involvement were reported to be rare, 0.1% and 0.5–4%, respectively. Spine involvement has been reported in 50% of patients with bone involvement.
Case Report: We presented a rare case of an 18-year-old male patient with a recurrent mediastinal hydatid cyst which widened the neural foramina, extended into the spinal canal, and compressed the spinal cord. He presented with back pain, spastic paraparesis, and bowel/bladder incontinence. Computed tomography (CT) and magnetic resonance imaging (MRI) showed polycystic mediastinal mass with erosion of the upper thoracic vertebra and the rib; widening of the neural foramina; extension into the spinal canal and compression of the spinal cord. The patient was operated on. Through a posterior approach, the polycystic mass was removed totally. The mass in the mediastinal (paravertebral) area was removed totally through the widened neural foramen. The cavity was washed with 3% hydrogen peroxide. The histopathology confirmed the diagnosis of a hydatid cyst. Postoperatively the patient was treated with oral albendazole for six months. On the sixth month follow-up, the neurologic status had only mild improvement and the follow-up scan did not show any recurrence of the infection.
Conclusion: Hydatid cysts can rarely involve the mediastinal (paravertebral) area and can extend to the spinal epidural space causing neurologic compromise.
Keywords: Dumbbell tumor, Hydatid cyst, Mediastinum, Spine
INTRODUCTION
Hydatid disease, or echinococcosis, is a parasitic infection of humans caused by tapeworms of the genus Echinococcus. Echinococcosis is caused by ingestion of food, water contaminated by the parasite egg or close contact with the infected animal host [1]. Dogs and other carnivore animals are the definitive hosts for the cycle while omnivores and herbivores like sheep, goats, pigs, and rodents (for the Alveolar) are the intermediate hosts. Humans are so-called accidental hosts [1]. The liver and lungs are the most common organs to be involved. Mediastinal and bone involvement were reported to be rare, 0.1% and 0.5–2%, respectively [2],[3]. Vertebral involvement accounts for 50% of the patients with hydatid cyst of the bone [4]. The thoracic region is the region most affected by the spine, followed by the lumbar region [3]. There have been less than 15 cases of mediastinal hydatid cysts with vertebral erosion and intraspinal extension [5]. The pathophysiology of the mediastinal involvement is speculated to be either lymphatic or arterial dissemination through the aortic branch [6],[7]. The treatment is based on extensive surgery combined with anthelmintic therapy. Irrigating the surgical field with scolicidal agents like 3% hypertonic saline, 3% hydrogen peroxide, and cetrimide may help prevent recurrence [8]. Albendazole is the anthelmintic drug of choice for the treatment of hydatid cysts [9].
A cure has not been achieved yet, and recurrences needing reoperation are reported in most cases [3].
CASE REPORT
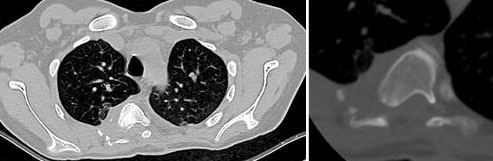
This is an 18-year-old male patient who presented with upper back pain radiating to the left chest, progressive lower extremity weakness of three years duration, and associated urinary and fecal incontinence of the same duration. He had the same history seven years ago, for which he was operated on and improved completely. He was ambulatory for four years. He didn’t come for medical follow-up after the first surgery and his biopsy result from the first surgery was not able to be found in his records. Up on neurologic examination, motor power in the upper extremity was 5/5, and lower extremity motor power was 0/5 on the right and 1/5 on the left. Reflex was +2 on the biceps and triceps and +4 on the patella and ankle, hypertonic lower extremity, and normotonic upper extremity. The sense of pain and temperature was intact, but the sense of pressure and vibration was lost in the deep tendons of the lower extremity. Upon digital rectal examination, there was lax anal tone, absent voluntary anal grip, absent perianal sensation, and a positive bulbocavernosus reflex. Chest X-ray showed right upper lung field and paraspinal homogeneous circular opacity (Figure 1). On cervicothoracic MRI, there was a T3–T4 level paraspinal mass involving the vertebral body. The T4 vertebral body was partially eroded by the mass and the mass extended to the epidural space and posterior mediastinum (Figure 2). Computed tomography scan showed a mediastinal multicystic mass with neural foraminal widening and extension of the mass into the spinal canal at the level (Figure 3).
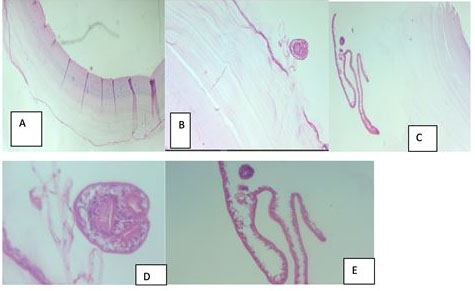
After informed consent, the patient was taken to the operating room (OR) and under general anesthesia (GA) put in a prone position. T3–T4 hemi-laminectomy was performed, exposing through a midline vertical incision T3–T4. An epidural mass was found with extensive adhesion to the dura. The mass had an outer encasing capsule and small multiple cysts inside (Figure 4 and Figure 5). There was a rupture of the outer cyst intraoperatively. The mediastinal component of the cysts was removed through the widened neural foramina. After total removal of the cysts, the cavity was washed with 3% hydrogen peroxide. Histopathologic examination of the mass revealed cyst wall fragments featuring a laminated outer layer and inner germinal membrane, which is typical of a hydatid cyst (Figure 6). On the second postoperative day, patient’s lower extremity power became 2/5 on all key muscle groups. Postoperative CT scan images done on the second postoperative day demonstrates complete excision. The patient was treated with oral albendazole after surgery, which is continued for six months. He has been on outpatient follow-up for the last six months. On the sixth months visit his lower extremity motor power was 2/5 on all key muscle groups. The CT scan on sixth month follow-up didn’t show recurrence (Figure 7).
DISCUSSION
Hydatid cyst is prevalent in sheep-raising countries. The infestation occurs in direct contact with dogs or from contaminated water and food. The cysts migrate to different organs through the bloodstream, mainly through the portal venous system, mostly to the liver (60–70%) and the lung (10–15%). Involvement of other organs is not common [10]. The first spine hydatid cyst was described by Churrier in 1807. Hydatid cysts can cause spinal cord compression from vertebral, paraspinal with foraminal extension (dumbbell type), primary epidural, intradural, and intramedullary origin lesions. Braithwaite and Lees classified spinal hydatid cysts into paraspinal, spinal, and intraspinal, where intraspinal lesions are further divided into extradural, intradural extramedullary, or intramedullary [11]. Spinal hydatid cyst most commonly affects the thoracic level (52%) followed by lumbar (37%), cervical (5.5%), and sacral spine (5.5%) [12]. The spinal hydatid cyst grows 1–5 cm per year and often causing cord compression.
Among the different types of spinal hydatid cysts, intradural extramedullary and intramedullary types are very rare with few case reports. Vertebral hydatid cyst accounts for 0.5–2% of all hydatid cyst cases and 50% of hydatid cyst of the bone [4],[13],[14].
Vertebral echinococcosis occurs after hydatid embryos reach the vertebrae through various portals. The cyst grows by expanding along the diverticulum within the trabecular space, infiltrating the bone as it progresses, and destroying it. The extraosseous stage begins with resorption of bone tissue and perforation of the cortex and periosteum. Paraspinal and spinal canal extension cause spinal cord compression [15]. Although there are reports in pediatric age groups, it usually affects those 30–50 years of age. Within the spine, the thoracic spine is affected in most cases, followed by the lumbar and sacral spines. It rarely involves the cervical spine. The disease usually begins in the center of the vertebral body, with a preference for the pedicle, and the disc space is resistant. In the spinal canal, it can involve the extradural space or intradural extramedullary or intramedullary space, the latter being very rare. The cysts can be single or multiple. They may give rise to secondary cysts by micro-ruptures [10].
A mediastinal hydatid cyst is a rare form of hydatid disease. Hydatid cysts in the mediastinal and paravertebral locations account 0.1% of all cases [16]. From the mediastinal hydatid cysts, 45% of cysts were located in the posterior mediastinum, 36% in the anterior mediastinum, and 18% in the middle mediastinum [17]. Hydatid cysts in this location can mimic other congenital and neoplastic conditions. The differentials include bronchogenic cyst, thymic cyst, enteric cyst, pericardial cyst, and cystic teratoma [18]. Hydatid cysts involving the posterior mediastinum and the paravertebral location can extend the spinal canal and cause cord compression [5]. In mediastinal/paravertebral hydatid cysts the vertebral body can be scalloped or eroded and there could be widened neural foramen in cases with a spinal canal extension [19]. There have been less than 10 cases of mediastinal hydatid cysts with spinal canal extension reported [5],[19],[20],[21],[22],[23],[24].
Patients usually present with insidious onset back pain and different degrees of motor power weakness, sensory loss, and bowel/bladder disturbances. Since this is how most spine and spinal cord pathologies present. A high index of suspicion is required to reach to diagnosis.
Serologic tests such as eosinophilia and a positive result of the complement fixation test, a Casoni skin test, and an enzyme-linked immunoassay help to establish the diagnosis of a spine hydatid cyst [25].
On histopathology, a hydatid cyst consists of three layers; a peripheral adventitial layer, which is fibrous tissue containing many eosinophils, an intermediate cuticular layer characterized by amorphous, densely staining laminated chitinous material, and an inner germinal layer that has nucleated epithelium [26].
Plain film, anterior-posterior (AP) and lateral, may show homogenous opacity in the posterior mediastinum. Evidence of spinal canal extension might be remarked by an increased interpedicular distance, pedicle deformation, and posterior scalloping of the vertebral body [5]. A CT scan will help to see bone erosions, the paraspinal extension, and the involvement of the paraspinal structures. Magnetic resonance imaging is the preferred imaging in evaluation of spinal hydatid cysts. It can show the extent of lesions and spinal cord compression. On spinal MRI, hydatid cyst mostly appears as cystic with walls that are thin and regular. The cyst walls appear markedly hypointense on T1-weighted and T2-weighted images and with an absence of wall enhancement with gadolinium. Diffusion-weighted MRI can help differentiate complicated hydatidosis from other cystic lesions [12].
The preferred treatment for hydatid cysts is en bloc excision without rupture of the cyst followed by systemic anthelmintic medication. Puncture and aspiration of the cyst can be helpful in cases that are difficult to achieve radical resection [27]. Unlike hydatid cysts in other organs of our body, spinal hydatid cysts are found to be invasive and multiple. They are intimately in contact with the spinal cord and roots, making their en bloc removal challenging. Rupturing the cyst may cause anaphylaxis and dissemination of the infection. When there are multiple cysts in different areas of the spine, surgery should be performed on the one causing cord or root compression and making the patient symptomatic [28]. Most reports recommend giving albendazole or mebendazole to these patients [5]. Albendazole has good oral absorption that blocks glucose uptake and depletes glycogen stores, immobilizing and killing the parasite, and the side effect is hepatotoxicity. Mebendazole has poor gastrointestinal (GI) absorption, hence, requiring a high dose and may cause neutropenia [15]. The recommendation is to give the anthelmintic medication preoperatively to decrease cyst size, reduce the risk of rupture, and increase the rate of radical resection. It is also recommended to continue the medication postoperatively to prevent recurrence and dissemination. There is no consensus on how long to continue. After the first surgery, it is recommended to continue anthelmintic medication for 3–12 months and for recurrences to continue indefinitely. The dosage regimen based on the World Health Organization (WHO) recommendations for visceral hydatidosis is (15 mg/kg/day) in two divided doses [29]. A good response to treatment is demonstrated on follow-up MRI by cyst shrinkage, calcification, or remaining stable over one year [15]. Intraoperatively, irrigating the field using scolicidal agents such as 3% hydrogen peroxide, povidone-iodine, 10% formaldehyde, and 0.5% silver nitrate has been recommended to reduce anaphylaxis, prevent dissemination, and prolong and prevent recurrence [8]. Although a recurrence rate of 30–100% has been reported in the literature, surgery gives an acceptable quality of life with prolonged survival [10]. The need for fusion and what type of fusion material to use—autologous or synthetic—is not clear yet. Therefore, the decision is based on expert experience and surgeons’ preferences [30]. Morbidity and mortality are high in recurrence surgeries [28].
CONCLUSION
Mediastinal hydatid cyst with spinal canal extension is a very rare form of echinococcosis that can mimic various mediastinal cystic lesions. It should be considered as a differential in the appropriate epidemiologic setting. The mainstay of treatment is surgical excision with anthelmintic medication. If it is not managed early it can lead to severe neurologic compromise.
REFERENCE
1.
Kern P, Menezes da Silva A, Akhan O, et al. The Echinococcoses: Diagnosis, clinical management and burden of disease. Adv Parasitol 2017;96:259–369. [CrossRef]
[Pubmed]

2.
Kabiri el H, al Aziz S, el Maslout A, Benosman A. Hydatid cyst: An unusual disease of the mediastinum. Acta Chir Belg 2001;101(6):283–6.
[Pubmed]

3.
Işlekel S, Zileli M, Erşahin Y. Intradural spinal hydatid cysts. Eur Spine J 1998;7(2):162–4. [CrossRef]
[Pubmed]

4.
Manenti G, Censi M, Pizzicannella G, et al. Vertebral hydatid cyst infection. A case report. Radiol Case Rep 2020;15(5):523–7. [CrossRef]
[Pubmed]

5.
Kumar S, Satija B, Mittal MK, Thukral BB. Unusual mediastinal dumbbell tumor mimicking an aggressive malignancy. J Clin Imaging Sci 2012;2:67. [CrossRef]
[Pubmed]

6.
Tadasa S, Dencha B, Gebrekidan M, Bedasso S, Tsehay Abebe A. Posterior mediastinal hydatid cyst with spine and chest wall involvement. Int Med Case Rep J 2023;16:371–6. [CrossRef]
[Pubmed]

7.
Isitmangil T, Toker A, Sebit S, Erdik O, Tunc H, Gorur R. A novel terminology and dissemination theory for a subgroup of intrathoracic extrapulmonary hydatid cysts. Med Hypotheses 2003;61(1):68–71. [CrossRef]
[Pubmed]

8.
Besim H, Karayalçin K, Hamamci O, Güngör C, Korkmaz A. Scolicidal agents in hydatid cyst surgery. HPB Surg 1998;10(6):347–51. [CrossRef]
[Pubmed]

9.
10.
Turgut M. Hydatid disease of the spine: A survey study from Turkey. Infection 1997;25(4):221–6. [CrossRef]
[Pubmed]

11.
Braithwaite PA, Lees RF. Vertebral hydatid disease: Radiological assessment. Radiology 1981;140(3):763–6. [CrossRef]
[Pubmed]

12.
Padayachy LC, Ozek MM. Hydatid disease of the brain and spine. Childs Nerv Syst 2023;39(3):751–8. [CrossRef]
[Pubmed]

13.
Dagtekin A, Koseoglu A, Kara E, et al. Unusual location of hydatid cysts in pediatric patients. Pediatr Neurosurg 2009;45(5):379–83. [CrossRef]
[Pubmed]

14.
Dogan I, Kahilogullari G, Guner E, Unlu A. A rare and unexpected clinical progress and location on a primary extradural spinal hydatid cyst in a pediatric patient: A case report. Childs Nerv Syst 2015;31(8):1407–11. [CrossRef]
[Pubmed]

15.
Zhang Z, Fan J, Dang Y, Xu R, Shen C. Primary intramedullary hydatid cyst: A case report and literature review. Eur Spine J 2017;26(Suppl 1):107–10. [CrossRef]
[Pubmed]

16.
Eroğlu A, Kürkçüoğlu C, Karaoğlanoğlu N, Tekinbaş C, Kaynar H, Onbaş O. Primary hydatid cysts of the mediastinum. Eur J Cardiothorac Surg 2002;22(4):599–601. [CrossRef]
[Pubmed]

17.
Traibi A, Atoini F, Zidane A, Arsalane A, Kabiri El H. Mediastinal hydatid cyst. J Chin Med Assoc 2010;73(1):3–7. [CrossRef]
[Pubmed]

18.
Esme H, Eren S, Sezer M, Solak O. Primary mediastinal cysts: Clinical evaluation and surgical results of 32 cases. Tex Heart Inst J 2011;38(4):371–4.
[Pubmed]

19.
Karakasli A, Yilmaz M, Mucuoglu AO, Yurt A. A large primary dumbbell hydatid cyst causing neural foraminal widening of the thoracic spine: A case report and literature review. Int J Surg Case Rep 2015;8C:55–8. [CrossRef]
[Pubmed]

20.
Tian Y, Jiang M, Shi X, Hao Y, Jiang L. Case report: Huge dumbbell-shaped primary hydatid cyst across the intervertebral foramen. Front Neurol 2020;11:592316. [CrossRef]
[Pubmed]

21.
Zairi M, Boussetta R, Msakni A, Sahraoui G, Mohseni AA, Nessib MN. Infected primary hydatid cyst of the right lumbar paraspinal muscles: A rare case in a ten-year-old child. Int J Surg Case Rep 2021;89:106570. [CrossRef]
[Pubmed]

22.
Dighe MP, Balasubramaniam S, Nadkarni TD. Transthoracic approach for ventrally situated paraspinal extradural hydatid cyst of the dorsal spine. J Craniovertebr Junction Spine 2018;9(4):271–3. [CrossRef]
[Pubmed]

23.
Xu X, Cao J, Wang J, Wu T, Xu P. A rare case of recurrent primary dumbbell-shaped spinal hydatidosis. Radiol Case Rep 2022;17(9):3224–7. [CrossRef]
[Pubmed]

24.
Kassimi M, Rami A, Habi J, et al. Recurrent costovertebral hydatidosis with epidural extension. Radiol Case Rep 2021;16(7):1712–4. [CrossRef]
[Pubmed]

25.
Awasthy N, Chand K. Primary hydatid disease of the spine: An unusual case. Br J Neurosurg 2005;19(5):425–7. [CrossRef]
[Pubmed]

26.
Senol MG, Tekeli H, Kendirli MT, et al. Intramedullary hydatid cyst of the cervical spine. Indian J Med Microbiol 2012;30(4):480–1. [CrossRef]
[Pubmed]

27.
Bozbuga M, Celikoglu E, Boran BO. Hydatid cyst of the craniocervical junction: Case report. Neurosurgery 2005;57(1):E193 [CrossRef]
[Pubmed]

28.
Arif SH, Zaheer S. Intradural extramedullary primary hydatid cyst of the spine in a child: A very rare presentation. Eur Spine J 2009;18(Suppl 2):179–82. [CrossRef]
[Pubmed]

29.
Echinococcosis. [Available at: https://www.who.int/health-topics/echinococcosis]

30.
Gopal N, Chauhan S, Yogesh N. Primary spinal extradural hydatid cyst causing spinal cord compression. Indian J Orthop 2007;41(1):76–8. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Abraham Tadele - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Endris Hussen - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Biniam Gebreegziabher - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Fasil Mesfin - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2024 Abraham Tadele et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.