|
Case Report
Heterotopic pregnancy and the influence of letrozole
1 Medical Student, Department of Basic Biomedical Sciences, Touro College of Osteopathic Medicine, 60 Prospect Ave, Middletown, NY 10940, USA
2 Attending Physician, Department of Obstetrics and Gynecology, Vassar Brothers Medical Center, 45 Reade Pl, Poughkeepsie, NY 12601, USA
3 Attending Physician, Department of Obstetrics, Optum Health, 2515 South Rd, Poughkeepsie, NY 12601, USA
4 Attending Physician, Department of Family Medicine, Esopus Medical PC, 120 Maple Ridge Drive, Ulster Park, NY 12487, USA
Address correspondence to:
Adele El Kareh
MD, PhD, FACOG, MS, 2507 South Road-Route 9, Poughkeepsie, NY 12601,
USA
Message to Corresponding Author
Article ID: 100126Z06LO2024
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Ocampo L, Bahrampour S, Pincinato PH, Bray A, El Kareh A, Maas AL. Heterotopic pregnancy and the influence of letrozole. Case Rep Int 2024;13(1):7–11.ABSTRACT
Introduction: Heterotopic pregnancy has become increasingly common following increased use of assisted reproductive techniques. We will examine one uncommon instance of a heterotopic pregnancy occurring in the setting of a young woman undergoing letrozole therapy for primary infertility, making it an uncommonly seen case.
Case Report: We report a young otherwise healthy female G1P0 at approximately 6 weeks gestation, who was referred from her primary care office to the Emergency Department with progressive abdominal pain that started 12 hours prior and had started to exhibit signs of hemodynamic instability. History was significant for difficulty with conception requiring letrozole treatment. Emergency laparoscopy was performed and confirmed additional ectopic pregnancy in the right fallopian tube with blood originating from the fimbriated end. Evacuation of hemoperitoneum and removal of ectopic pregnancy was completed without complication. She was discharged from the hospital in stable condition.
Conclusion: In any woman of reproductive age presenting with lower abdominal pain or abnormal bleeding, there should be a strong suspicion for a pregnancy until confirmed otherwise. These patients may benefit from prompt imaging with pelvic ultrasound to assist in earlier detection of ectopic embryo implantation and, subsequently, earlier intervention. Salpingectomy, ideally via laparoscopic approach, remains the gold standard for diagnosis and treatment of patients with a ruptured ectopic pregnancy in the setting of a heterotopic pregnancy, although surgical intervention is associated with poorer outcomes for the intrauterine pregnancy.
Keywords: Ectopic pregnancy, Heterotopic pregnancy, Letrozole, Obstetrics, Public health, Reproductive health
INTRODUCTION
Heterotopic pregnancy is a life-threatening condition in which intrauterine and extrauterine gestations occur simultaneously. It has become increasingly common throughout the years, and this case presentation examines one instance of a heterotopic pregnancy occurring in the setting of a young woman receiving letrozole therapy for primary infertility to augment ovulation.
When a fertilized ovum grows into the blastocyst stage, it begins the process of implantation in the uterine cavity, and the developing embryo is guided by several factors, including the influence of estrogen and progesterone on the endometrial tissue, beaconing of numerous cytokines, and the integrity of the Fallopian tubes and uterus itself to ensure smooth passage [1]. When the balance of any of these factors are disrupted, it can lead to complications, one of which is heterotopic pregnancy.
Risk factors for a heterotopic pregnancy include tubal scarring, especially following pelvic inflammatory disease (PID), endometriosis, malformations of the uterus, ovarian hyperstimulation syndrome, and multiple embryo transfer during in vitro fertilization (IVF) [2],[3].
In this case presentation, the effects of letrozole therapy will be examined. Previous studies have shown that drugs like clomiphene citrate, used to treat infertility via ovarian stimulation, are linked to heterotopic pregnancies [3]. The mechanism by which clomiphene citrate leads to ovarian stimulation relies on the rapid rate of follicular maturation augmented by the upregulation of follicle-stimulating hormone (FSH) receptors and FSH release from the pituitary [4]. Letrozole, an aromatase inhibitor, works similarly by blocking the conversion of androgens into estrogen, which causes a subsequent increase in FSH, encouraging the growth and development of multiple follicles in the ovaries of women who are seeking fertility treatment [5]. Theoretically, since letrozole stimulates ovulation there is an increased risk of multiple gestation, and by default an increased risk of heterotopic pregnancy [6]. Interestingly, despite this theoretical risk, only one other case of heterotopic pregnancy has been documented in a patient with letrozole augmentation, making this a noteworthy exhibition [7].
CASE REPORT
A 28-year-old otherwise healthy female G1P0 at approximately six weeks gestation was referred from the office to the Emergency Department for severe, progressive abdominal pain of 12 hours duration. She denied vaginal bleeding or fever. No nausea, vomiting, diarrhea, or urinary symptoms were reported. History was significant for hyperprolactinemia treated with three months of cabergoline with subsequent normalization of serum prolactin, benign phyllodes tumor of the left breast resected 10 years ago, and difficulty with conception despite normal prolactin levels and luteal phase progesterone. The patient opted for a trial of letrozole to augment 102 ovulation and conceived on her sixth cycle. Besides letrozole, the patient did not use 103 any other medications for ovulation induction, ovulation triggers, or luteal phase support 104 medications.
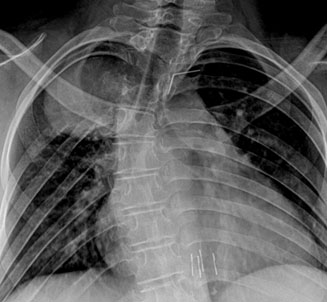
While in the ED waiting room, she had a syncopal episode and lost consciousness for about 30 seconds. Vital signs were stable on arrival, with a normal temperature, a mildly elevated heart rate of 97 bpm, and blood pressure of 119/68. Examination of the abdomen revealed generalized tenderness with rebound and guarding, mild distention, and hypoactive bowel sounds. Laboratory studies were significant for an elevated white blood cell count of 17.1 × 109/L, and a low hemoglobin and hematocrit of 10.1 mg/L and 29.3 mL/L, respectively. Compared to labs drawn one month prior, hemoglobin and hematocrit were significantly decreased indicating recent blood loss. Serum beta human chorionic gonadotropin (HCG) was 30,094 U/L. Transvaginal ultrasound (TVUS) revealed an intrauterine pregnancy (IUP) with a crown rump length of 0.5 cm, normal amniotic fluid levels, a fetal heart rate of 119 bpm (Figure 1) and moderate complex free pelvic fluid. A large complex mass about 9 cm was seen adjacent to the right ovary (Figure 2), as well as a small amount of complex fluid in the uterus (Figure 3) and a cyst in the left adnexa (Figure 4).
Emergency laparoscopy was performed under general anesthesia. More than 1200 cc of clotted blood was evacuated from the peritoneal cavity (Figure 5) and an ectopic embryo was confirmed to be in the right fallopian tube (Figure 5) with blood originating from the fimbriated end. Also noted was a left paratubal cyst (Figure 6).
Right salpingectomy was performed along with removal of the cystic cavity on the left. Hemostasis was confirmed and thorough irrigation was performed. Post-operative ultrasound confirmed a viable IUP with fetal heart rate of 126 bpm. Specimens were sent to pathology and histological examination of the presumed ectopic pregnancy confirmed chorionic villi consistent with our diagnosis.
The patient remained hospitalized an additional day because of a persistently elevated white blood count without fever. The post-operative course was otherwise uncomplicated. The patient was discharged from the hospital on post-operative day 2 in stable condition, with a viable 6-week IUP.
DISCUSSION
Assisted Reproductive Techniques (ARTs) and IVF are becoming increasingly popular for the modern family hoping to conceive. Statistics show that 42% of average Americans know someone or are personally going through a form of fertility treatment [8]. Women with a history of, or currently undergoing ART (which includes those taking medications for ovulation induction, follicle stimulating hormones, or who are undergoing IVF) are at a significantly higher risk for heterotopic pregnancy, defined as multiple gestations with one being intrauterine and the other being extrauterine (ovaries, fallopian tube, and rarely in abdomen) [9]. Most commonly, and in our patient’s case, the second pregnancy occurred in the fallopian tube. Patients undergoing ART or IVF are at a higher risk of heterotopic pregnancy of about 1/100 to 1/500, as compared to the risk in the natural conception population of 1/30 000 [9]. In addition to the added risk, it is also more difficult to diagnose in this population due to the enlarged ovaries which can mask an ectopic pregnancy [10].
Nevertheless, as previously noted, no statistics or risk analysis is yet available regarding patients undergoing letrozole therapy specifically. Only a single case has been documented.
This is unexpected, theoretically, as the probability of multiple pregnancies increases, so does the probability of developing a heterotopic pregnancy.
As the population of women undergoing ART and/or IVF continues to increase, there should be a high index of suspicion for heterotopic pregnancy in females of childbearing age who present with lower abdominal pain or abnormal vaginal bleeding. Even if there is confirmed IUP, thorough exam of bilateral ovaries and fallopian tubes via transvaginal ultrasound should be completed in addition to serial serum beta HCG. Nabi et al. preferred TVUS compared to transabdominal ultrasound and suggested that if exams are inconclusive, high resolution TVUS or even magnetic resonance imaging (MRI) could be employed [11]. One might also consider taking into 160 consideration an elevated white blood cell (WBC), which was recorded in our case and several others, such as those described by Madžarac et al., who recorded a WBC of 31.8 × 109/L, and Cerniauskaite et al., who described a WBC of 18.11 × 109/L [6],[12].
We propose the use of early ultrasound examinations for patients who are undergoing infertility treatment to increase the chance of earlier detection and subsequent intervention. The majority of cases are caught in the 5–8 weeks range and are usually due to concern for a ruptured ectopic pregnancy, which can be life-threatening [9],[13]. Earlier detection may help in avoiding emergency surgery, which not only puts the patient at risk of post-surgical complications but increases the risk of loss of the IUP. More conservative treatments include ultrasound-guided aspiration, or feticide injection with potassium chloride or hyperosmolar glucose [14].
These more conservative treatments cannot be employed if there is any suspicion of rupture or hemodynamic instability and require expertise. Surgical intervention remains the gold standard of diagnosis and treatment in patients with suspicion of rupture; it is the best way to visualize the ovaries and fallopian tubes, remove the ectopic pregnancy, and evacuate any free pelvic fluid. Although surgical intervention is associated with poorer outcomes for the IUP, it was necessary in our case because of her presentation with acute abdomen and hemodynamic instability.
Thankfully, our patient was discharged on post-operative day 2 with a viable 6-week pregnancy, and she continues to do well, now in her second trimester.
CONCLUSION
Frequency of ectopic pregnancy is increased in patients undergoing in vitro fertilization. This case report highlights a heterotopic pregnancy with ruptured ectopic at six weeks gestation in a 28-year-old female with no significant past medical history, who was taking letrozole for primary infertility. Emergent laparoscopy under general anesthesia was performed as both a diagnostic and therapeutic measure. This procedure confirmed a ruptured right ectopic pregnancy as well as a viable intrauterine pregnancy. Based on this patient’s case presentation, and the literature underlying the relationship between supplemental fertility treatments and ectopic pregnancy, patients undergoing IVF, ART, or ovulation augmentation with letrozole or clomiphene may benefit from routine screening ultrasound examinations to assist in early detection.
REFERENCE
1.
Su RW, Fazleabas AT. Implantation and establishment of pregnancy in human and nonhuman primates. Adv Anat Embryol Cell Biol 2015;216:189–213. [CrossRef]
[Pubmed]

2.
Liu M, Zhang X, Geng L, et al. Risk factors and early predictors for heterotopic pregnancy after in vitro fertilization. PLoS One 2015;10(10):e0139146. [CrossRef]
[Pubmed]

3.
Maleki A, Khalid N, Rajesh Patel C, El-Mahdi E. The rising incidence of heterotopic pregnancy: Current perspectives and associations with in-vitro fertilization. Eur J Obstet Gynecol Reprod Biol 2021;266:138–44. [CrossRef]
[Pubmed]

4.
Samsonia MD, Lesnovskaia EE, Kandelaki MA. Clomiphene, ovarian hyperstimulation syndrome and pregnancy. [Article in Russian]. Georgian Med News 2009;(166):26–9.
[Pubmed]

5.
Yang AM, Cui N, Sun YF, Hao GM. Letrozole for female infertility. Front Endocrinol (Lausanne) 2021;12:676133. [CrossRef]
[Pubmed]

6.
Madžarac V, Duić Ž, Valetić J, Planinić-Radoš G. In-vitro fertilization resulting in heterotopic pregnancy, ovarian hyperstimulation and paralytic ileus: A case report. Case Rep Womens Health 2019;22:e00106. [CrossRef]
[Pubmed]

7.
Vargas RA, Leal R, Tijerina LO, Sepulveda DL. Heterotopic pregnancy: A case report. J Minim Invasive Gynecol 2015;22(6S):S138. [CrossRef]
[Pubmed]

8.
Usage of fertility treatment among adults by income U.S. 2023. (n.d.). Statista. Retrieved February 29, 2024. [Available at: https://www.statista.com/statistics/1416647/usage-of-fertility-treatment-among-adults-by-income/]

9.
Tal J, Haddad S, Gordon N, Timor-Tritsch I. Heterotopic pregnancy after ovulation induction and assisted reproductive technologies: A literature review from 1971 to 1993. Fertil Steril 1996;66(1):1–12. [CrossRef]
[Pubmed]

10.
Hassani KIM, Bouazzaoui AE, Khatouf M, Mazaz K. Heterotopic pregnancy: A diagnosis we should suspect more often. J Emerg Trauma Shock 2010;3(3):304. [CrossRef]
[Pubmed]

11.
Nabi U, Yousaf A, Ghaffar F, Sajid S, Ahmed MMH. Heterotopic pregnancy – A diagnostic challenge. Six case reports and literature review. Cureus 2019;11(11):e6080. [CrossRef]
[Pubmed]

12.
Černiauskaitė M, Vaigauskaitė B, Ramašauskaitė D, Šilkūnas M. Spontaneous heterotopic pregnancy: Case report and literature review. Medicina (Kaunas) 2020;56(8):365. [CrossRef]
[Pubmed]

13.
Ouafidi B, Kiram H, Benaguida H, Lamrissi A, Fichtali K, Bouhya S. Diagnosis and management of a spontaneous heterotopic pregnancy: Rare case report. Int J Surg Case Rep 2021;84:106184. [CrossRef]
[Pubmed]

14.
Li JB, Kong LZ, Yang JB, et al. Management of heterotopic pregnancy: Experience from 1 tertiary medical center. Medicine (Baltimore) 2016;95(5):e2570. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Lovingly Ocampo - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Sheeva Bahrampour - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Pietra Herrero Pincinato - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Adeline Bray - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Adele El Kareh - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Amelia Lisa Maas - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2024 Lovingly Ocampo et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.