|
Case Report
Intravenous leiomyomatosis: A rare case report
1 General Surgery Center, Yankuang New Journey General Hospital, Zoucheng, Shandong 273500, China
Address correspondence to:
Zheng Xiuhai
General Surgery Center, Yankuang New Journey General Hospital, Zoucheng, Shandong 273500,
China
Message to Corresponding Author
Article ID: 100128Z06ZX2024
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Xiuhai Z, Yadong L, Suai T, Dekai M. Intravenous leiomyomatosis: A rare case report. Case Rep Int 2024;13(2):1–4.ABSTRACT
Introduction: Intravascular leiomyomatosis (IVL) is a rare histological benign tumor without invading the tissue of the venous vessels themselves. It is characterized by continuous intraluminal growth of benign smooth muscle tumor cells along with the uterine vein to the pelvic and abdominal venous systems, including the iliac vein and inferior vena cava, and even to the right atrium of the heart and pulmonary artery, leading to life-threatening complications. This case report describes a 43-year-old female patient with IVL who underwent four myomectomy surgeries.
Case Report: A 43-year-old female patient with rare IVL was admitted after four myomectomy surgeries. After preoperative evaluation by color Doppler ultrasound, cardiac ultrasound, chest and abdominal computed tomography (CT) scans, this patient underwent total hysterectomy, bilateral salpingectomy, and complete resection of the entire intravascular leiomyoma. This article discusses the characteristics, diagnosis, treatment, and especially surgical precautions of IVL. In addition to surgical resection, this article also discusses other treatment options for IVL.
Conclusion: Intravascular leiomyomatosis has unique biological characteristics and clinical manifestations. Through accurate diagnosis and timely complete tumor resection, as well as regular follow-up after surgery, most IVL patients can achieve good long-term prognosis and quality of life. However, further research is needed on the etiology and pathogenesis of IVL.
Keywords: Diagnosis, Intravenous leiomyomatosis, Surgery
INTRODUCTION
Intravascular leiomyomatosis (IVL) is a rare histological benign tumor without invading the tissue of the venous vessels themselves. It is characterized by continuous intraluminal growth of benign smooth muscle tumor cells along the uterine vein to the pelvic and abdominal venous systems, including the iliac vein and inferior vena cava, and even to the right atrium of the heart and pulmonary artery, leading to life-threatening complications [1],[2],[3],[4],[5]. There are still many challenges in the clinical diagnosis and treatment of IVL. Complete tumor resection including IVL is necessary [6]. Herein, we report a case of IVL in a 43-year-old female patient who underwent four myomectomy procedures, and reviewed the progress of IVL in recent years.
CASE REPORT
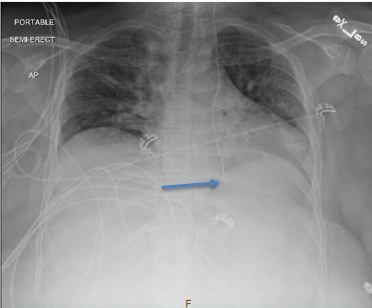
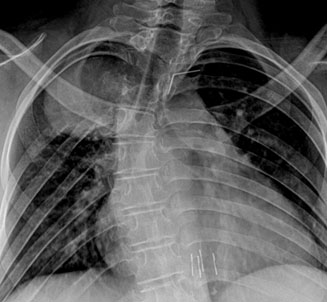
A 43-year-old female patient was admitted to the hospital on January 29, 2024 due to the discovery of a pelvic mass during regular physical examination. She had no abdominal pain, no fever, no abnormal bowel and bowel movements, no abnormal vaginal bleeding, and no significant weight gain or loss during the course of the disease. She had underwent uterine leiomyoma removal surgeries four times in 2011, 2012, 2013, and 2022, and denied having a family history of similar diseases. She was checked by color Doppler ultrasound after admission to our hospital, which showed abnormal hypoechogenicity in the uterus, suggesting the possibility of uterine leiomyoma imaging. There is a hypoechoic nodule between the uterus and ovary, suggesting the possibility of leiomyoma, as shown in Figure 1A. Pelvic CT examination showed: The uterine morphology is irregular, with intrauterine device shadows and low-density shadows in the left adnexal area, as shown in Figure 1B. Cardiac ultrasound, chest and abdominal CT did not reveal any significant abnormalities or special features. After preoperative evaluation upon admission, a total hysterectomy and bilateral salpingectomy were performed. During the surgery, it was observed that the uterus had an irregular shape, a slightly hard texture, a size of about 7 × 5 × 4 cm, adhesion to the bladder and sigmoid colon, widening of the bilateral cervical isthmus, extending toward the broad ligament, and palpable mass on the left side. The texture was soft, with unclear borders, and the lifting was in a bead like shape, located within the vascular sheath. It extended toward the pelvic wall, with a complete capsule, running along the iliac blood vessels. The vascular wall was cut open, and the tumor was peeled off from the vascular wall. When approaching the proximal end of the tumor, the tumor was gently pulled out, and the proximal end of the cardiovascular segment was sutured. The size of the intravascular tumor is approximately 15 × 5 × 3 cm, with a soft, grayish white texture and a flower shaped tail end. The boundary is smooth, as shown in Figure 1C. Intraoperative frozen section pathology showed leiomyoma with individual atypical cells detected. Postoperative pathology showed multiple nodules in the uterine muscle layer, with a diameter of 0.5–1 cm, which were leiomyomas. In the intravascular specimen, a leiomyoma was identified (Figure 1D).
DISCUSSION
Intravascular leiomyomatosis was first described by Birsch-Hirschfeld in 1896 [7]. As of 2022, only 748 IVL patients have been reported [6]. Case reports and small case series still dominate. Intravascular leiomyomatosis mainly invades the systemic venous circulation through the uterine iliac vein and ovarian vein [1]. 0.97% of patients with hysteromyoma were diagnosed with IVL, 54.3% of the IVL patients had intracardiac involvement, and 13.5% involved the pulmonary artery [8].
The etiology responsible for the proliferation of IVL is not yet clear [9],[10],[11],[12]. Dal Cin et al. suggested that a specific chromosomal aberration, the presence of an extra copy of 12q15qter and/or the loss of 14q24-qter may be a critical genetic event leading to intravascular intrusion and proliferation [13]. After comparing differentially expressed genes (DEGs) between IVL and common uterine leiomyomas, Wang et al. found that genes related to angiogenesis and anti-apoptotic pathways may play a crucial role in the development and pathogenesis of IVL [14].
Common clinical symptoms of IVL include abdominal pain, pelvic mass, and abnormal vaginal bleeding. When the tumor spreads to the heart or pulmonary artery, there may be swelling in the lower limbs, chest discomfort, shortness of breath, and fainting. However, approximately 20–30% of IVL patients have no symptoms [15]. Echocardiography, abdominal ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) can help diagnose and determine the degree of tumor invasion. However, it is difficult to see small smooth muscle tumors in small blood vessels, especially in early patients.
Surgical resection is the main treatment option for IVL. Complete resection is key point to reduce recurrence [16]. Bin Li et al. reported complete surgical resection of tumors with a recurrence rate of almost 0%, while incomplete resection resulted in one-third of patients experiencing recurrence [17]. These results indicate that surgical residues are an important cause of postoperative recurrence, which may be related to the failure to correctly diagnose or detect early invasive vascular lesions during the first surgery [18]. In order to avoid residual tumor rupture in blood vessels during surgery, it is necessary to accurately estimate the location of tumor invasion into blood vessels before surgery. During the surgical process, it is necessary to locate the distal end and perform gentle surgery along the vine shaped intravascular tumor. Sometimes, a combination of open vascular surgery and endovascular techniques is required to completely and safely remove the tumor from the affected vein. When the tension of the traction leiomyoma is high, it is necessary to open the blood vessels, remove the tumor inside the blood vessels, and pay attention to the continuity of the tumor. It is very important to confirm the complete distal end of the intravascular tumor. Usually, the complete distal end presents as a smooth and clear tumor boundary. If the tumor ruptures and remains, the tumor will recurrence, while severe cases may result in distal tumor detachment, leading to venous embolism and endangering life. If the lesion invades the internal iliac vein and inferior vena cava, a multidisciplinary team consisting of surgeons, interventional radiologists, and vascular specialists may be required to achieve complete resection [19]. In this patient’s surgery, gentle traction was performed on the distal end of the tumor, followed by incision of the internal iliac vein. Finally, when approaching the proximal end of the tumor, the tumor can be gently pulled out. The smooth boundary of the distal end of the tumor was checked to confirm complete resection.
If surgical resection is not feasible or the tumor is too large, other treatment options such as radiation therapy or embolization can be considered. These treatments can help shrink tumors and alleviate symptoms, but they are usually not curable [20],[21]. According to the report by Zhang et al., sirolimus is safe and effective in treating recurrent cases [22]. Considering the high expression of estrogen receptor (ER) and progesterone receptor (PR) in IVL patients, hormone therapy is widely used [23],[24]. However, research has found that in cases which IVL resection is incomplete, postoperative use of antiestrogen therapy does not reduce the recurrence rate [17].
The estimated recurrence rate of IVL is about 16.6–30%, mainly due to the large tumor volume, insufficient understanding of the disease, and incomplete surgical resection [18],[25],[26]. Due to the complex clinical manifestations and biological behavior of IVL, long-term regular follow-up after surgery is crucial, regardless of whether surgery is performed or not. Close follow-up and monitoring can help detect tumor recurrence and control related symptoms. If possible, for patients with IVL recurrence, reoperation is a better option [27].
CONCLUSION
In summary, IVL has unique biological characteristics and clinical manifestations. Through accurate diagnosis and timely complete tumor resection, as well as regular follow-up after surgery, most IVL patients can achieve good long-term prognosis and quality of life. However, further research is needed on the etiology and pathogenesis of IVL.
REFERENCE
1.
Zhou X, Qi X, Zhao X, Yang F. Update on clinical characteristics and molecular insights for uterine intravenous leiomyomatosis (Review). Oncol Lett 2023;27(1):31. [CrossRef]
[Pubmed]

2.
He G, Yao T, Zhao L, et al. Surgical strategy for intravenous leiomyomatosis spreading from uterine to the right atrium presenting with recurrent syncope. J Cardiothorac Surg 2024;19(1):209. [CrossRef]
[Pubmed]

3.
Dai DQ, Wang SL, Xiao D, Huang ZC, Tang GC. A rare case of intravenous leiomyomatosis extending to inferior vena cava. Am J Med Sci 2024:S0002-9629(24)01118-2. [CrossRef]
[Pubmed]

4.
Kikuchi DS, Goulbourne CA, Starbuck KD, Fernandes MF. Case report: Intravenous leiomyomatosis with intracaval and intracardiac growth. Eur Heart J Case Rep 2022;7(1):ytac464. [CrossRef]
[Pubmed]

5.
Cohen D, Mordhorst A, Misskey J, Jamieson A, Faulds J. Surgical management of intravenous leiomyomatosis with intracardiac extension. J Vasc Surg Cases Innov Tech 2023;9(4):101302. [CrossRef]
[Pubmed]

6.
Lim WH, Lamaro VP, Sivagnanam V. Manifestation and management of intravenous leiomyomatosis: A systematic review of the literature. Surg Oncol 2022;45:101879. [CrossRef]
[Pubmed]

8.
Wei JL, Ji X, Zhang P, Chen WJ, Zhao YN, Liu M. Complete intravenous leiomyomatosis: A case report and literature review. Ann Palliat Med 2021;10(11):12039–45. [CrossRef]
[Pubmed]

9.
Ge Z, Feng P, Zhang Z, Liang Z, Chen R, Li J. Identification of novel serum protein biomarkers in the context of 3P medicine for intravenous leiomyomatosis: A data-independent acquisition mass spectrometry-based proteomics study. EPMA J 2023;14(4):613–29. [CrossRef]
[Pubmed]

10.
Tamura S, Hayashi T, Tokunaga H, Yaegashi N, Abiko K, Konishi I. Oncological properties of intravenous leiomyomatosis: Involvement of mesenchymal tumor stem-like cells. Curr Issues Mol Biol 2021;43(2):1188–202. [CrossRef]
[Pubmed]

11.
Hayashi T, Yaegashi N, Konishi I. Molecular pathological approach of uterine intravenous leiomyomatosis. Ann Transl Med 2022;10(13):724. [CrossRef]
[Pubmed]

12.
Ordulu Z, Nucci MR, Dal Cin P, et al. Intravenous leiomyomatosis: An unusual intermediate between benign and malignant uterine smooth muscle tumors. Mod Pathol 2016;29(5):500–10. [CrossRef]
[Pubmed]

13.
Dal Cin P, Quade BJ, Neskey DM, Kleinman MS, Weremowicz S, Morton CC. Intravenous leiomyomatosis is characterized by a der(14) t(12;14)(q15;q24). Genes Chromosomes Cancer 2003;36(2):205–6. [CrossRef]
[Pubmed]

14.
Wang W, Wang Y, Chen F, et al. Intravenous leiomyomatosis is inclined to a solid entity different from uterine leiomyoma based on RNA-seq analysis with RT-qPCR validation. Cancer Med 2020;9(13):4581–92. [CrossRef]
[Pubmed]

15.
Kiliç S, Çinar T, Çiçek V, et al. Intravenous leiomyomatosis with intracardiac extension as a rare cause of abdominal pain in an adult patient: A case report. J Tehran Heart Cent 2021;16(4):178–81. [CrossRef]
[Pubmed]

16.
Magdalena P, Thomas B, Nina P, et al. Successful one-stage resection of intracardiac intravenous leiomyomatosis: A case report. Gynecol Oncol Rep 2023;48:101243. [CrossRef]
[Pubmed]

17.
Li B, Chen X, Chu YD, Li RY, Li WD, Ni YM. Intracardiac leiomyomatosis: A comprehensive analysis of 194 cases. Interact Cardiovasc Thorac Surg 2013;17(1):132–8. [CrossRef]
[Pubmed]

18.
Zhang G, Yu X, Lang J, Liu B, Zhao D. Analysis of risk factors for post-operative recurrence or progression of intravenous leiomyomatosis. Int J Gynecol Cancer 2024;34(5):705–12. [CrossRef]
[Pubmed]

19.
Wang Q, Liu H, Feng W. Unraveling the challenges of intravenous leiomyomatosis: A retrospective analysis of 11 cases. Arch Gynecol Obstet 2024;309(2):621–9. [CrossRef]
[Pubmed]

20.
Mizoguchi C, Matsumoto H, Nasu K, Arakane M, Kai K, Narahara H. Intravenous leiomyomatosis treated with radical hysterectomy and adjuvant aromatase inhibitor therapy. J Obstet Gynaecol Res 2016;42(10):1405–8. [CrossRef]
[Pubmed]

21.
Murphy AN, Byrne D, Salati U, Lawler L. Intravenous leiomyomatosis manifesting as saddle embolism. BMJ Case Rep 2019;12(3):e228267. [CrossRef]
[Pubmed]

22.
Zhang G, Fan R, Yang H, et al. Safety and efficacy of sirolimus in recurrent intravenous leiomyomatosis, pulmonary benign metastatic leiomyomatosis, and leiomyomatosis peritonealis disseminata: A pilot study. BMC Med 2024;22(1):119. [CrossRef]
[Pubmed]

23.
Biri A, Korucuoglu U, Zumrutbas N, Tiras B, Guner H. Intravenous leiomyomatosis treated with aromatase inhibitor therapy. Int J Gynaecol Obstet 2008;101(3):299–300. [CrossRef]
[Pubmed]

24.
Wu CK, Luo JL, Yang CY, et al. Intravenous leiomyomatosis with intracardiac extension. Intern Med 2009;48(12):997–1001. [CrossRef]
[Pubmed]

25.
Moniaga NC, Randall LM. Uterine leiomyomatosis with intracaval and intracardiac extension. Gynecol Oncol Case Rep 2012;2(4):130–2. [CrossRef]
[Pubmed]

26.
Du J, Zhao X, Guo D, Li H, Sun B. Intravenous leiomyomatosis of the uterus: A clinicopathologic study of 18 cases, with emphasis on early diagnosis and appropriate treatment strategies. Hum Pathol 2011;42(9):1240–6. [CrossRef]
[Pubmed]

27.
Peng J, Zhong F, Zhu Y, et al. Clinical analysis of uterine intravenous leiomyomatosis: A retrospective study of 260 cases. J Obstet Gynaecol Res 2021;47(12):4357–64. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Zheng Xiuhai - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Li Yadong - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Tan Suai - Acquisition of data, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Meng Dekai - Acquisition of data, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2024 Zheng Xiuhai et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.