|
Case Series
Endoscopic versus surgical management in Bouveret’s syndrome: A case series
1 General Surgery Resident, General Surgery Department, ULS Alentejo Central, Évora, Portugal
2 General Surgery Consultant, General Surgery Department, ULS Alentejo Central, Évora, Portugal
3 Head of Department of General Surgery, General Surgery Department, ULS Alentejo Central, Évora, Portugal
Address correspondence to:
Joana Simões Bolota
ULS Alentejo Central, Largo do Senhor da Pobreza, 7000-811 Évora,
Portugal
Message to Corresponding Author
Article ID: 100129Z06JB2024
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Bolota J, Leandro S, Cotovio M, Cinza M, Senhorinho R, Carvalho M. Endoscopic versus surgical management in Bouveret’s syndrome: A case series. Case Rep Int 2024;13(2):5–10.ABSTRACT
Introduction: Bouveret’s syndrome is a rare entity, accounting for 1–3% of gallstone ileus cases. It is more common in elderly females and is associated with significant morbidity and mortality. It presents with epigastric pain, nausea, and vomiting in patients with concurrent cholelithiasis. Given the nonspecific symptoms, the diagnosis is supported with imaging highlighting Rigler’s triad. The therapeutic approach can be either endoscopic or surgical.
Case Series: The authors present two cases of Bouveret’s syndrome, managed with two different approaches. The first case is an 82-year-old man presenting with diffuse abdominal pain and distension, nausea, and vomiting. Blood tests showed increased inflammatory parameters and an abdominal computed tomography (CT) scan compatible with Bouveret’s syndrome. Upper gastrointestinal (GI) endoscopy revealed a fistula at D2 level, and an obstruction at D3, caused by a 3 cm gallstone. The patient underwent laser and mechanical lithotripsy for gallstone removal. The second case is a 71-year-old woman presenting with vomiting associated with dehydration and abdominal pain for several days. Blood tests showed increased inflammatory parameters and CT scan showed a bilioduodenal fistula at D2 level, with a 5 cm a gallstone at that level, confirmed in the endoscopy. An attempt to remove the gallstone was performed, without success, so the patient underwent laparotomy with extraction of the gallstone via an anterior gastrotomy.
Conclusion: Bouveret’s syndrome is a rare disease that requires thoughtful and tailored management. Given this rarity, there is minimal data to support specific therapy recommendations. Therefore, management should be tailored to the patient at the discretion of the multidisciplinary team and the resources of the institution.
Keywords: Bouveret’s syndrome, Cholecystoduodenal fistula, Cholelithiasis, Endoscopic lithotripsy
INTRODUCTION
Bouveret’s syndrome is described as an obstruction of the duodenal lumen caused by the migration of a gallstone through a cholecystogastric or a cholecystoduodenal fistula [1],[2],[3],[4],[5],[6],[7],[8]. It is a rare entity, accounting for 1–3% of gallstone ileus cases [7],[8], being more common in elderly females, with a median age of 74 years old and associated with significant morbidity (around 30–40%) and mortality (up to 12%) due to significant patient comorbidities [1],[2],[3],[4]. This syndrome usually presents with epigastric pain, nausea, and vomiting in patients with concurrent cholelithiasis. Given the nonspecific symptoms, the diagnosis requires a high suspicion level and is supported with imaging that usually highlights the Rigler’s triad of pneumobilia, gastrointestinal obstruction, and ectopic gallstone [3],[4],[8]. The therapeutic approach can be either endoscopic or surgical, and the selection of the most suitable technique will depend on the obstruction characteristics, patient factors and means available in each center [1],[4],[7].
The authors present two cases of Bouveret’s syndrome, with two different approaches according to the patient’s clinical status, highlighting both endoscopic and surgical treatment.
CASE SERIES
Case 1
An 82-year-old man presented in the emergency department with a 5-day history of abdominal pain, nausea, and multiple episodes of intermittent bilious vomiting.
The patient had a background history of aortic valve prosthesis due to aortic stenosis, AVB grade I, diabetes mellitus, hypertension, and hypercholesterolemia. On admission, he was hemodynamically stable, and physical examination revealed a distended abdomen, diffusely painful at palpation, without peritoneal signs. Blood tests showed raised white blood cell counts (WBCs) 20×109/L, and C-reactive protein (CRP) was 17 mg/L.
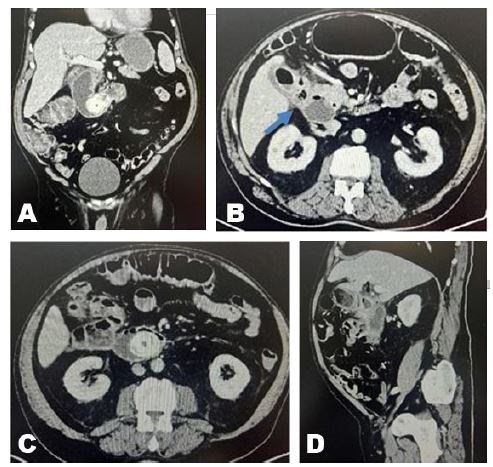
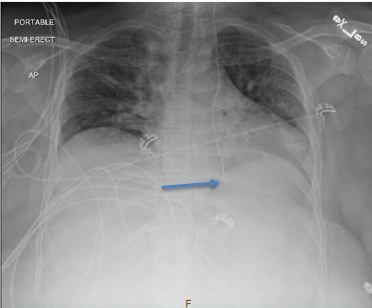
An urgent computed tomography (CT) scan of the abdomen and pelvis showed “duodenal obstruction by a gallstone with 43×30 mm, with important distention of the stomach and first three portions of the duodenum, due to cholecystoduodenal fistulization, with wall thickness and some free air. There were also signs of pneumobilia on the common bile duct” (Figure 1A, Figure 1B, Figure 1C, Figure 1D).
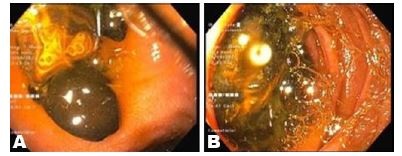
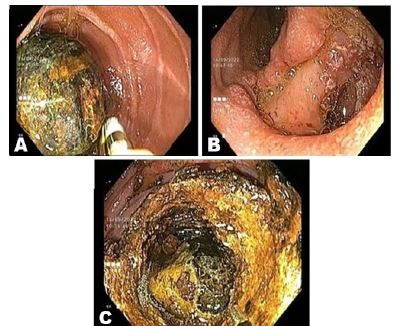
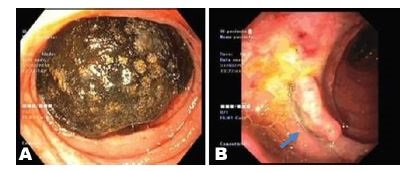
The patient started intravenous fluids and broad spectrum antibiotic, and underwent nasogastric decompression, followed by an urgent upper gastrointestinal (GI) endoscopy, that revealed several small gallstones. A small opening with some ulceration was identified as the fistula at D2 level. At D3 level, a larger, 3 cm diameter, hard gallstone was identified and tried to remove, without success (Figure 2A and Figure 2B). Since lithotripsy was not available, the patient was transferred to another center, where he underwent laser lithotripsy complemented with mechanical lithotripsy. The stone fragments were retrieved into the gastric lumen with the lithotripsy basket and Roth net, and successfully removed (Figure 3A, Figure 3B, Figure 3C).
The patient recovered uneventfully, and blood reports gradually became normal after the endoscopy. He was discharged seven days after admission. Since then, the patient has been well, with no abdominal pain, in a 26-month follow-up period.
Case 2
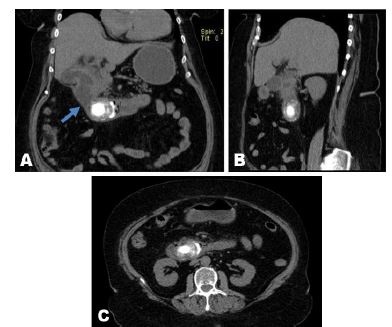
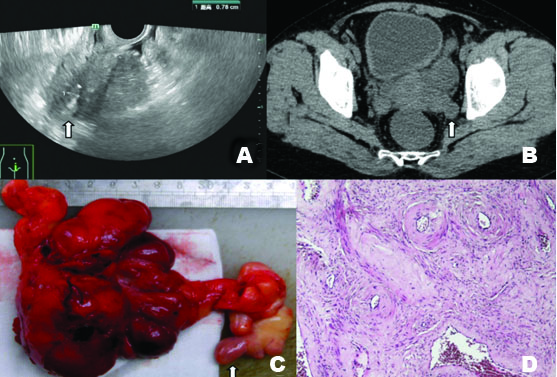
71-year-old woman with a recent admission on hospital for Mallory–Weiss syndrome and diagnosed with cholecystoduodenal fistula, presented in the emergency department with persistent vomiting associated with abdominal pain for several days. She had a background history of hypertension, diabetes mellitus, chronic heart failure, hypothyroidism, and obesity-hypoventilation syndrome. On admission, the patient was dehydrated, and a tender upper abdomen was noted. Blood tests showed raised WBCs 23×109/L, and CRP 43 mg/L. Computed tomography scan of the abdomen and pelvis showed a biliodigestive fistula between the gallbladder infundibulum and D2 level, and a 5 cm gallstone at D2 level leading to a significant gastric distention (Figure 4A, Figure 4B, Figure 4C).
The patient started intravenous fluids, antiemetic, and underwent nasogastric decompression. An endoscopy was performed, which confirmed a bilioduodenal fistula and a 5 cm stone impacted on D2 level. An attempt to remove the gallstone was performed, without success (Figure 5A and Figure 5B).
A laparotomy was proposed, with the stone being extracted using an anterior gastrotomy. The immediate postoperative period was complicated with a global respiratory insufficiency, in the context of acute illness in a patient with previous severe respiratory and cardiovascular comorbidities, needing mechanical ventilation and intensive care unit (ICU) admission for 36 h, with favorable evolution. On 5th postoperative day, the patient developed a surgical wound infection, treated with drainage and antibiotics. The patient was discharged on the 21st postoperative day, and has been asymptomatic since then, in a 60 months follow-up.
DISCUSSION
Bouveret’s syndrome consists of an obstruction of the duodenal lumen or gastric antrum caused by the migration of a gallstone through a bilioduodenal or biliogastric fistula [1],[2],[3],[4],[5],[6],[7],[8]. It is a rare entity, corresponding to 1–3% of all cases of gallstone ileus, and is more prevalent in the elderly and females, with a reported median age of incidence of 74 years old and a female-to-male ratio of 1:9 [1],[2],[3],[4].
Gallstone ileus occurs in 0.3–5% of patients presenting with cholelithiasis, due to the development of bilioenteric fistulas. Impacted gallstones can range from 2 to 10 cm, and, most frequently, ileus occurs with stones larger than 2.5 cm [1],[7],[8]. The fistula usually forms in pressure zones between the gallbladder/bile duct and the digestive tract, after chronic inflammation. The obstruction causes increased intraluminal pressure that leads to local ischemia and necrosis, allowing the gallstone to perforate the walls and pass into the bowel [1],[3],[4],[5]. Malignancy and anatomical changes due to previous surgery can also cause fistulization and stone migration. Some studies report a relationship between the presence of juxtapapillary duodenal diverticula (JPDD) and an increased risk of cholecystolithiasis and choledocholithiasis, therefore, indirectly, it may be a risk factor for Bouveret syndrome [1],[9].
Differential diagnoses include perforated peptic ulcer, erosive gastritis, gastric volvulus, bezoars, Mirizzi syndrome, duodenal carcinoma, cholangiocarcinoma, and duodenal web [1],[3],[4]. The morbidity and mortality are due to significant associated patient comorbidities, which can be less if there is an early diagnosis and more restrictive surgery [3],[6],[8].
Clinical presentation depends on the degree of obstruction, and impaction site of the stone. It usually presents with a triad of epigastric pain, nausea, and vomiting, but other symptoms may also be present, including abdominal pain, distension, upper gastrointestinal bleeding, fever, weight loss, and anorexia. Physical examination usually reveals dehydration and abdominal distension and tenderness [3],[4],[8].
As clinical signs and symptoms are nonspecific and variable, it is important to associate them with imaging studies. Rigler’s triad is one of the most common features, consisting of pneumobilia, small-bowel obstruction, and an ectopic radio-opaque gallstone [1],[2],[7]. Plain X-ray can be the first line imaging study, but it has low sensitivity (21%). Abdominal ultrasound can show the pneumobilia and the ectopic stone but sometimes it is difficult due to intestinal gas [1],[3]. Computed tomography scan has good sensitivity and specificity (93% and 100% respectively). The best imaging technique for identifying Rigler’s triad, which is specific to gallstone ileus, can also show the exact location of the obstruction [4],[7],[8]. Magnetic resonance cholangiopancreatography (MRCP) can also be used to help find the fistulas and concrements. More invasive diagnostic techniques include esophagogastroduodenoscopy (EGD) and surgery, both of which have diagnostic and therapeutic potential [2],[4],[7].
Treatment options for Bouveret’s syndrome include endoscopic management and surgery. The selection of the technique depends upon factors like the degree of obstruction, the impaction site, number, type, or size of gallstones, patient comorbidities, and clinical features at presentation, as well as expertise available, both endoscopic and surgical. Whenever possible, a multidisciplinary approach is encouraged [1],[4],[8].
Endoscopic treatment is considered the first line choice, as per many authors because it is the least invasive method, especially in older population with multiple comorbidities who may not otherwise tolerate the morbidity associated with surgery [2],[3],[6]. These treatments include direct endoscopic removal, mechanical lithotripsy, laser lithotripsy, extracorporeal shock wave lithotripsy, and intracorporeal electrohydraulic lithotripsy [1],[2],[8], and the success of these approaches relies on a good patient selection. Most of the stones implied in Bouveret’s syndrome are relatively large, measuring over 2.5 cm. Therefore, the risk of direct endoscopic removal is stone impaction in the esophagus, while fragmentation increases the risk of distal gallstone ileus. Other risks of endoscopic treatment include hemorrhage and perforation the intestinal wall [2],[4]. Despite some reports of success, 91% of patients will have to undergo surgery for definitive treatment [1],[4],[8].
The main treatment modality for Bouveret’s syndrome is surgery, especially when percutaneous or endoscopic approaches are not an option or have failed [3],[4],[7],[8]. The most common surgical options for extracting the stone are enterolithotomy and gastrotomy, performed either at the site of impaction or at a healthier segment. In cases of irreversible damage to small bowel wall, resection is required. Open and laparoscopic approaches are the most used techniques. However, when available, robotic surgery can minimize risks by improving visualization and allowing perform this procedure with a lower pneumoperitoneal pressures (8 mmHg), with benefits in minimizing cardiovascular compromise in this cohort of patients with significant comorbidities and acutely unwell, contributing to better outcomes [8]. Surgical treatment may be done in a one-stage procedure, with stone removal and simultaneous cholecystectomy, or in a two-stages procedure, with stone removal and later cholecystectomy and fistula repair [1],[4],[6],[7]. This decision is heavily influenced by the patient’s general condition, age, comorbidities, and current inflammatory status.
The cholecystectomy for retained gallstones and fistula repair prevents the subsequent cholecystitis and cholangitis. Some studies revealed that 10% of patients required reoperation with fistula repair due to persistent biliary symptoms [1],[4]. On the other hand, some authors claim that the fistula can close spontaneously if there are no residual stones in the gallbladder and the cystic duct is patent [1],[4],[8]. Younger patients with higher life expectancy seem more likely to develop secondary complications over time due to persistent bilioenteric fistula and would, thus, implicate simultaneous fistula repair in a one-stage procedure in case of acceptable health condition and absence of acute inflammatory state [3],[4],[6]. Laparoscopic and robotic techniques should be considered for surgical treatment whenever possible due to all the advantages associated with minimally invasive surgery. No data have shown which approach provides better outcomes, when applied to all cases.
Nonetheless, there still exists an important difference in success rates between endoscopic retrieval and surgical management (29% vs. 78% respectively) [1],[4],[7]. The authors suggest a tailored surgical strategy, adapted to each individual patient, when endoscopic treatment is not an option or has failed.
In the cases presented by the authors, therapeutic choices were made based on clinical status and resources available. Both patients underwent upper endoscopy as the first approach, failing in solving obstruction. In case 1, the patient was stable and lithotripsy was readily available, being the first choice and being able to remove the impacted gallstone. Unfortunately, in case 2, there was no possibility of urgent lithotripsy, so the patient was proposed to surgery via laparotomy, not being a candidate to a laparoscopic procedure due to comorbidities. In both cases presented by the authors, the gallbladder was left in place. In case 1, a patent cholecystoduodenal fistula was visualized with endoscopy. The patient was not fit for surgery, so he underwent MRCP, which showed no residual stones in the gallbladder and a patent cystic duct. In case 2, a clear fistulous tract between the duodenum and gallbladder was present. After the surgery, the patient was reevaluated, given the comorbidities and absence of symptoms, cholecystectomy was not proposed.
CONCLUSION
In conclusion, Bouveret’s syndrome is a rare disease that requires thoughtful and tailored management. Given this rarity, there are minimal data to support specific therapy recommendations. This case series enlightens different technical options to treat this condition—both endoscopic and surgical—that multidisciplinary teams must keep in mind when approaching these cases. Management should be tailored to the patient, considering all their comorbidities and clinical context, as well as the resources of available at the institution.
REFERENCE
1.
Nickel F, Müller-Eschner MM, Chu J, von Tengg-Kobligk H, Müller-Stich BP. Bouveret’s syndrome: Presentation of two cases with review of the literature and development of a surgical treatment strategy. BMC Surg 2013;13:33. [CrossRef]
[Pubmed]

2.
Dumonceau JM, Devière J. Novel treatment options for Bouveret’s syndrome: A comprehensive review of 61 cases of successful endoscopic treatment. Expert Rev Gastroenterol Hepatol 2016;10(11):1245–55. [CrossRef]
[Pubmed]

3.
Al-Habbal Y, Ng M, Bird D, McQuillan T, Al-Khaffaf H. Uncommon presentation of a common disease – Bouveret’s syndrome: A case report and systematic literature review. World J Gastrointest Surg 2017;9(1):25–36. [CrossRef]
[Pubmed]

4.
Haddad FG, Mansour W, Deeb L. Bouveret’s syndrome: Literature review. Cureus 2018;10(3):e2299. [CrossRef]
[Pubmed]

5.
Varre JS, Wu JL, Hopmann P, Ruiz O, Reddy R. Endoscopic and surgical management of Bouveret’s syndrome complicated by gallstone ileus. J Surg Case Rep 2021;2021(10):rjab464. [CrossRef]
[Pubmed]

6.
Shah FA, Winkle SM, Truitt T, Guez G, Draper K. Bouveret syndrome: A rare form of gallstone ileus. Cureus 2021;13(3):e14042. [CrossRef]
[Pubmed]

7.
Satchithanandha V, Lau NS, Galevska A, Sandroussi C. Bouveret syndrome: Two approaches one stone. J Surg Case Rep 2023;2023(10):rjad570. [CrossRef]
[Pubmed]

8.
Bhandari TR, Wong JLH, Ahmad J, Akbari K, Menon V. Bouveret’s syndrome: An old diagnosis. A modern multimodality approach (endoscopic and robotic surgical) of gastric outlet obstruction: Report of two cases. Int J Surg Case Rep 2024;114:109134. [CrossRef]
[Pubmed]

9.
Zoepf T, Zoepf DS, Arnold JC, Benz C, Riemann JF. The relationship between juxtapapillary duodenal diverticula and disorders of the biliopancreatic system: Analysis of 350 patients. Gastrointest Endosc 2001;54(1):56–61. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgement
The authors would like to thank Artur Silva, MD and Joana Oliveira, MD for their contributions to this article.
Author ContributionsJoana Simões Bolota - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Sofia Leandro - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Manuel Cotovio - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Margarida Cinza - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Rogério Senhorinho - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Manuel Carvalho - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2024 Joana Bolota et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.